Aseptic Techniques
A neurofeedback provider applied reusable EEG sensors to the scalp of a high school wrestler with skin lesions. When questioned, the wrestler explained that the lesions were due to mat abrasion and that all the wrestlers on his team had them. Since the clinician did not disinfect the sensors in between sessions, several of her clients developed MRSA infections and sued him for malpractice. This vignette was adapted from Moss (2013).

Neurofeedback providers may underestimate their risk of transmitting infection to their clients and may lack basic knowledge about risk mitigation strategies. Although clinicians may assume that infection risk is low since neurofeedback is noninvasive, handshakes, reclining chairs, cables, and sensors can easily transfer infectious organisms to clients. Moreover, over-abrasion in neurofeedback can expose sensors to client blood (Spaulding semi-critical classification), and inserted pelvic and rectal sensors expose sensors to tissue (Spaulding critical classification). This ubiquitous problem is called
common vehicle transmission.
Aseptic means free from disease-causing microorganisms. Aseptic techniques prevent contamination by harmful bacteria, viruses, or other microorganisms. Infection risk mitigation involves three strategies: handwashing and drying, disinfection of surfaces clients will contact, and disinfection or sterilization of sensors and cables (Hagedorn, 2014).
BCIA Blueprint Coverage
This unit covers
III Instrumentation and Electronics - D. Aseptic Techniques.

This unit covers Client and Trainer Hygiene, Screening, Hand Cleaning, Masks, Social Distance, Equipment Sterilization, Cross-Contamination, and Best Practices.
Please click on the podcast icon below to hear a full-length lecture.
CLIENT AND TRAINER HYGIENE
Moss and colleagues (2019) encourage clinicians to adopt a forensic perspective:
Think like a crime scene investigative agent. When you're working with a client, it is easy to touch the client, equipment, and workspace surfaces without awareness. If the client has a skin condition or even a cold, any object the practitioner touches in the environment can become a health hazard for the practitioner and for other clients. Restrict touching to a minimum and keep the things you touch in the same area, so they can be cleaned between clients. (pp. 338-339).
Screening
All staff should monitor their temperature and fever, respiratory symptoms, and other symptoms before leaving for work. Staff should administer the same symptom checklist before clients leave for the clinic. When clients arrive, take their forehead temperature using a contact-less infrared thermometer.
Graphic © Dimitry Naumov/Shutterstock.com.

Hand Cleaning
Upon arrival, staff should disinfect their hands with soap and water or a sanitizing product containing at least 60% isopropyl alcohol. CDC (2020) guidelines for handwashing include five steps:
- Wet your hands with clean, running water (warm or cold), turn off the tap, and apply soap.
- Lather your hands by rubbing them together with the soap. Lather the backs of your hands, between your fingers, and under your nails.
- Scrub your hands for at least 20 seconds. Need a timer? Hum the “Happy Birthday” song from beginning to end twice.
- Rinse your hands well under clean, running water.
- Dry your hands using a clean towel or air dry them.
Graphic © Black Duck Style/Shutterstock.com.

They should don disposable gloves and change them after training each client. Graphic © PENpicks Studio/Shutterstock.com.

Clients should disinfect their hands upon arrival with a sanitizing product. Both clients and staff should repeat this hand-cleaning process before leaving the clinic. Graphic © TRADOL/Shutterstock.com.

Masks
Staff should wear masks and face shields to protect themselves and their clients. They should provide disposable masks to clients who need them and require their use while in the clinic. Graphic © theskaman306/Shutterstock.com.

Social Distance
Remote neurofeedback training is the safest approach since clients remain at home. Clinicians should consider models that ensure the same quality of training as provided within a clinic. Graphic © Symphonic Mind Ltd.

If there are two doors, designate one as an entrance and another as an exit. Arrange the waiting area to exceed the minimum CDC recommended 6-ft (1.83-m) spacing between chairs. A plexiglass partition between reception staff and clients is desirable. Graphic © anon_tae/Shutterstock.com.

After skin preparation and cap or individual sensor placement, staff should interact with clients from the recommended distance or remotely from a control room.
EQUIPMENT STERILIZATION
Sterilization destroys all microbial life using chemical or physical methods. Disinfection by chemical agents or wet pasteurization removes many microorganisms except for bacterial spores on inanimate objects (CDC, 2020). With the exception of sensors that risk skin puncture and contact with blood, clinics will mainly mitigate infection using disinfectants.
Staff should wipe all surfaces that they or clients could touch with disinfectants like Freshnit®, Protex Disinfectant Spray®, or Virusolve®. These products are sporicidal and can destroy Clostridium difficile and methicillin-resistant Staphylococcus aureus. Products containing 20% isopropyl alcohol are ineffective against these pathogens (Hagedorn, 2019). Graphic courtesy of Bio-Medical Instruments.

Staff should use powerful disinfectants on sensors and leads applied to clients. Apply the product with a cloth and then remove excess with a wet cloth after a few minutes. Rinse the sensors, leads, and straps with lukewarm water, and air dry to minimize skin irritation. Never immerse sensors and leads in a cleaning product since this can damage them (Moss et al., 2019).
Despite the cost of disposable electrodes, they reduce the risk of infection transmission. Clinicians should dispose of them after each use because they may mistakenly apply them to a different client. Furthermore, their surfaces quickly degrade, compromising signal quality (Moss et al., 2019).
CROSS-CONTAMINATION
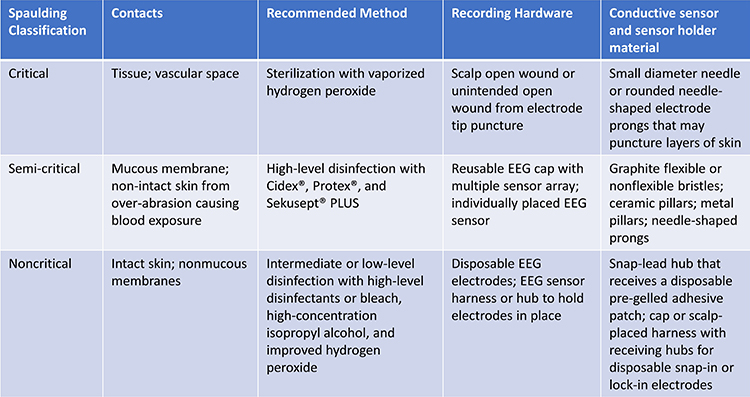
Cross-contamination is the inadvertent transfer of microorganisms from one individual or site to another. Infection mitigation should be guided by the Spaulding classification system for medical devices and sterilization (Rutala, Weber, & Healthcare Infection Control Practices Advisory Committee, 2008).
The Spaulding classification system identifies three levels of risk: critical, semi-critical, and noncritical. Neurofeedback caps and electrodes fall into the semi-critical and noncritical categories (Moss et al., 2019).
Critical means that sensors may breach the vascular space by puncturing the skin. Electrode prongs that can penetrate skin layers belong in this category and require sterilization. Vaporized hydrogen peroxide is a lower-temperature sterilization method that won't damage sensors like an autoclave or heat from 325-375 °F (Moss et al., 2019).
Semi-critical means that sensors can contact mucous membranes and blood due to skin abrasion. Reusable EEG cap sensors and individual sensors fall into this category and require high-level disinfection, destroying most microorganisms. Avoid abrasive cleaning products. Instead, use disinfectants like
"Cidex®, Protex®, and Sekusept® PLUS" (Moss, 2019, p. 340).
Noncritical means that the sensors can only contact non-mucous membranes and intact skin. Disposable EEG sensors and sensor hubs belong in this category and require intermediate or low-level disinfection. While high-level disinfectants may be used, bleach, high-concentration isopropyl alcohol, and improved hydrogen peroxide are effective cleaning agents (Moss et al., 2019).
The table below was slightly modified from Moss et al. (2019).
Best Practices
Skin Preparation
Current EEG amplifiers reduce the need for skin abrasion, increasing the risk of disease transmission by blood cells--even when blood is not visible. Ferree et al. (2001) discourage the use of blunt needles. If used, clinicians should discard them in a biohazard sharps container. After cleaning the skin with an alcohol pad, it can transmit infection and must be safely discarded without contacting common surfaces.
Do not apply abrasive gels like NuPrep with your gloved finger--use a cue tip instead. Discard each contaminated cue tip and use a new one to not contaminate the tube. Measuring tapes used to calculate head circumference present a noncritical risk and require low-level disinfection.
When transferring conductive gel
into a disposable plastic syringe, do not reinsert the blunt-tip needle into the gel container once it has touched you or the client.
Treat used blunt-tip needles, cue tips, tissues, and alcohol-impregnated wipes as biohazards and immediately safely discard them after use. Do not place them on a desk or tabletop where they can transmit disease (Moss, 2019).
Sensors
When clinicians place EEG sensors on abraded skin, this presents a semi-critical risk and requires high-level disinfectants like Cidex®, Protex™, and Sekusept® PLUS. When reusing EEG sensors, it is ideal only to reuse them with the same client.

Glossary
common vehicle transmission: a mode of transmission of infectious pathogens from a source that is common to all the cases of a specific disease.
critical: a Spaulding infection risk category for sensors that may breach the vascular space by puncturing the skin.
cross-contamination: the inadvertent transfer of microorganisms from one individual or site to another.
disinfection: a process involving chemical agents or wet pasteurization that removes many microorganisms except for bacterial spores on inanimate objects.
noncritical: a Spaulding infection risk category for sensors that can only contact non-mucous membranes and intact skin.
semi-critical: a Spaulding infection risk category for sensors that can contact mucous membranes and blood due to skin abrasion.
Spaulding classification system: a scheme that places reusable medical instruments or devices into three categories of ascending infection risk.
sterilization: a process that destroys all microbial life using chemical or physical methods.
TEST YOURSELF ON CLASSMARKER
Click on the Class Marker logo below to take a 10-question exam over this entire unit.

REVIEW FLASHCARDS ON QUIZLET
Click on the Quiz let logo to review our chapter flashcards.

Visit the BioSource Software Website
BioSource Software offers Physiological Psychology, which satisfies BCIA's Physiological Psychology requirement, and Neurofeedback100, which provides extensive multiple-choice testing over the Biofeedback Blueprint.

Assignment
Now that you have completed this module, identify ways to improve infection mitigation in your clinical practice.
References
Centers for Disease Control and Prevention (2020). Introduction, methods, definition of terms: Guideline for disinfection and sterilization in healthcare facilities (2008). Retrieved from https://www.cdc.gov/infectioncontrol/guidelines/disinfection/introduction.html.
Ferree, T. C., Luu, P., Russell, G. S., & Tucker, D. M. (2001). Scalp electrode impedance, infection risk, and EEG data quality. Clinical Neurophysiology, 112(3), 536–544. https://doi.org/10.1016/s1388-2457(00)00533-2
Hagedorn, D. (2019). Infection risk mitigation for biofeedback providers. In D. Moss & F. Shaffer (Eds.), Physiological recording technology and applications in biofeedback and neurofeedback (pp. 334-336). Association for Applied Psychophysiology and Biofeedback.
Moss, D., Hagedorn, D., Combatalade, D., & Neblett, R. (2019). Care for biofeedback and neurofeedback instrumentation.
In D. Moss & F. Shaffer (Eds.), Physiological recording technology and applications in biofeedback and neurofeedback (pp. 334-336). Association for Applied Psychophysiology and Biofeedback (pp. 337-347).
Rutala, W. A., Weber, D. J., & Healthcare Infection Control Practices Advisory Committee (2008). Guideline for disinfection and sterilization in healthcare facilities, 2008. Retrieved from www.cdc.gov/infectioncontrol/pdf/guidelines/disinfection-guidelines.pdf