Artifacting
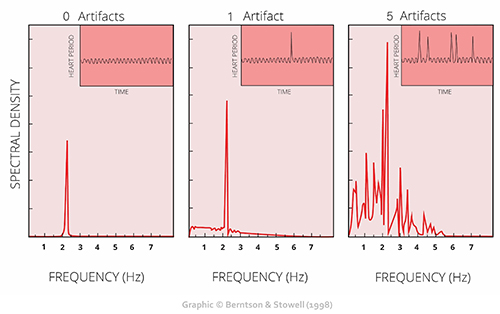
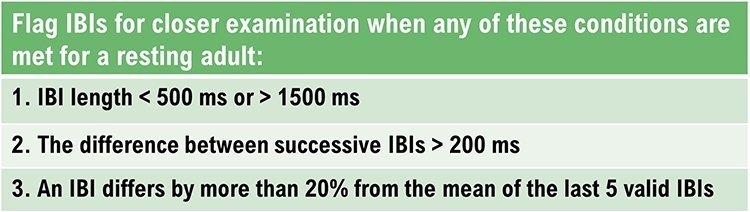
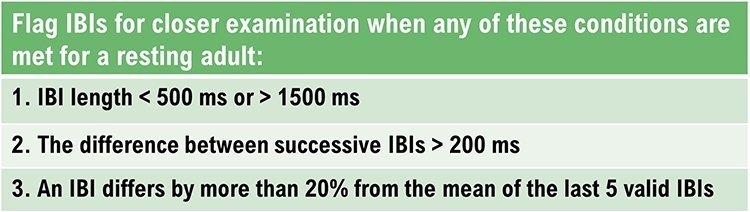
HRV recordings are vulnerable to diverse artifacts that can result in interbeat interval (IBI) values that are too long or too short.
Artifacts are false values produced by the client’s body (ectopic beats) and actions (movement), the environment (line current), and hardware limitations (light leakage).

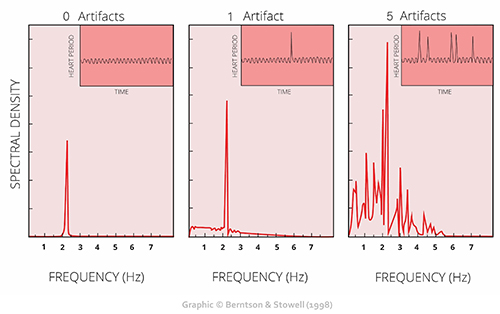
A single artifactual IBI value in a 2-minute epoch can markedly distort time-domain indices like SDNN (Berntson et al., 1997).
Client assessment and training are only as good as your data. © Scott Adams.
We recommend the “close the barn door before the horse escapes” strategy to ensure data integrity. Prevent artifacts before you record data so that you don’t have to remove it later.
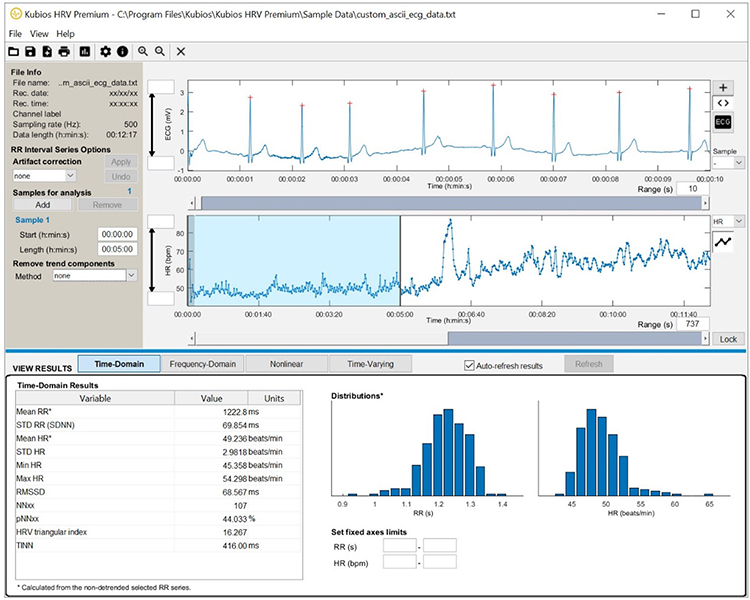
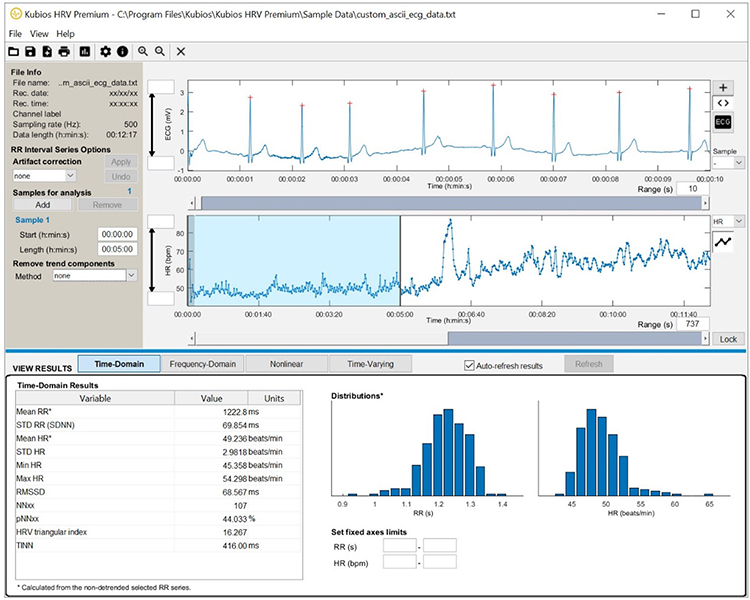
Manually inspect the raw signal and IBI values to ensure that artifacts do not contaminate your measurements. You can do this within free programs like Kubios or commercial programs like CardioPro Infiniti.
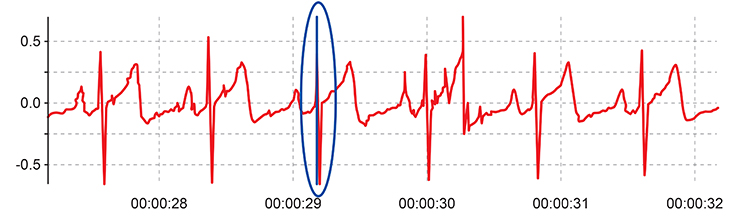
The relationship between artifacts in the raw signal and
false IBI values can be challenging for beginners to grasp. For ECG recording, the software analyzes the raw signal to measure the time intervals between consecutive R-spikes.
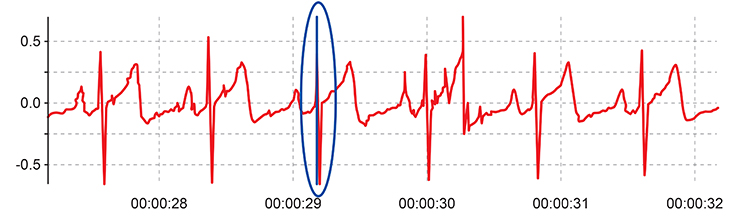
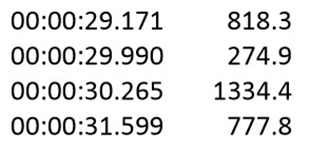
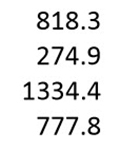
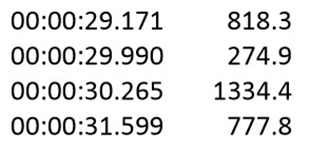
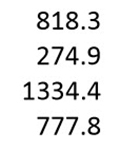
IBIs are stored in a time-stamped table of consecutive values. The ECG waveform circled above at 29.171 milliseconds corresponds to an IBI value of 818.359 milliseconds at the bottom of the table below.
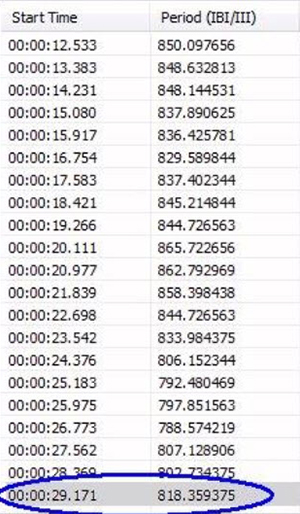
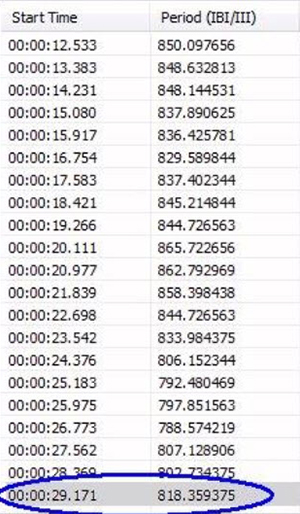
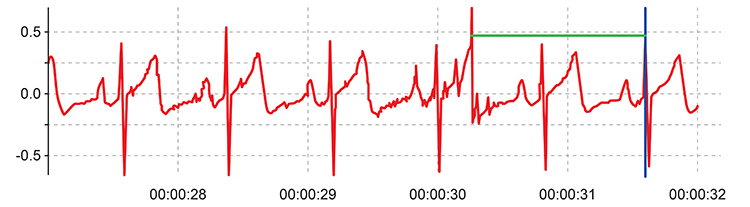
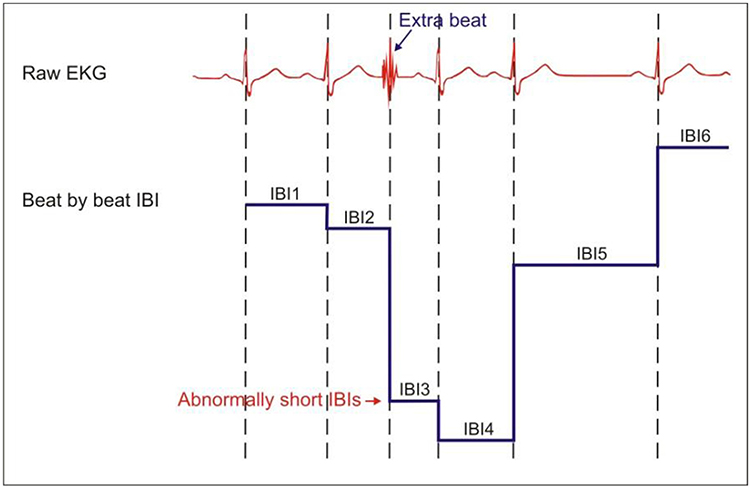
Artifacts can cause the software to "see" extra beats, resulting in short IBIs. They can also cause it to miss beats, resulting in long IBIs. The resulting IBI values stand out when you review a table of IBI values. For example, the green line identifies a short IBI of 274.9 milliseconds produced by an extra beat.
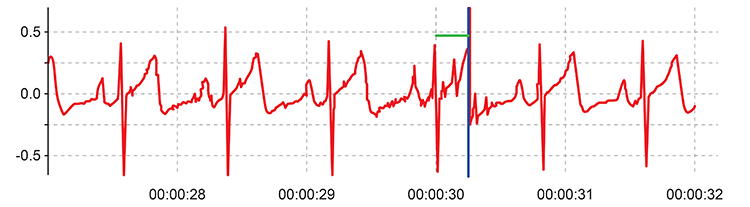
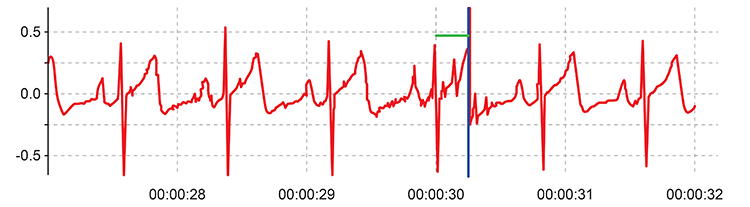
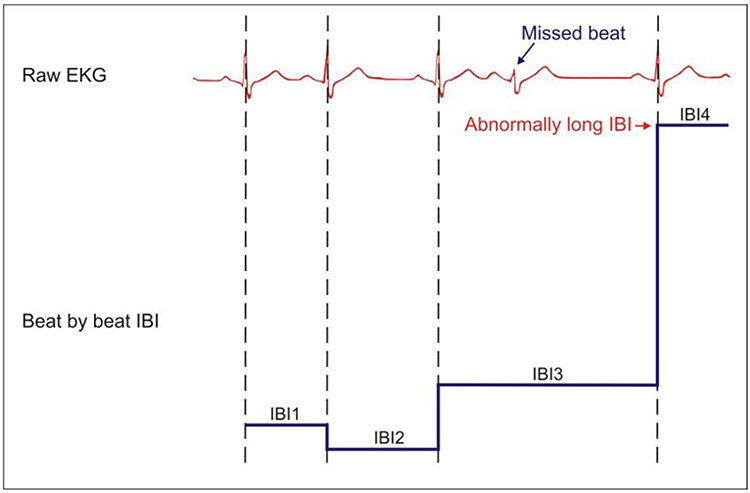
Next, the green line identifies a long IBI of 1334.4 milliseconds caused by a missed beat.
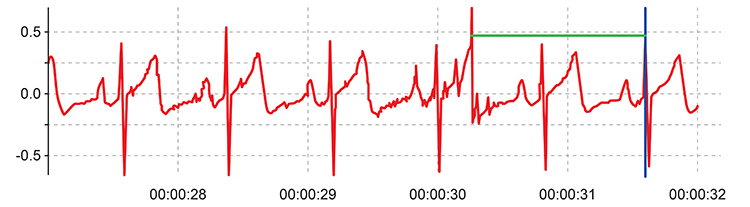
These short and long values stand out compared to typical values like 818.3 and 777.8.
BCIA Blueprint Coverage
This unit addresses
III. HRV Instrumentation: E. Artifacting Strategies.

This unit covers Artifacting Overview, Plan A: Segment Removal and Detrending, Plan B: Manual Correction and Detrending, Plan C: Automated Correction, and A Practical Perspective.
Please click on the podcast icon below to hear a full-length lecture.

Artifacting Overview
Artifacting is the process of removing or replacing false values found within a data record.

Researchers often have to discard the first and last minutes of data due to client adjustment to the monitoring environment and performance degradation after a long recording session.
Graphic © Vitaly Titov/Shutterstock.com.

Hack-and-Stitch Method
Never remove a part of an epoch and rejoin the remaining sections because this would distort the temporal relationship between heartbeats (Combatalade, 2010). Graphic © kagemusa/Shutterstock.com.

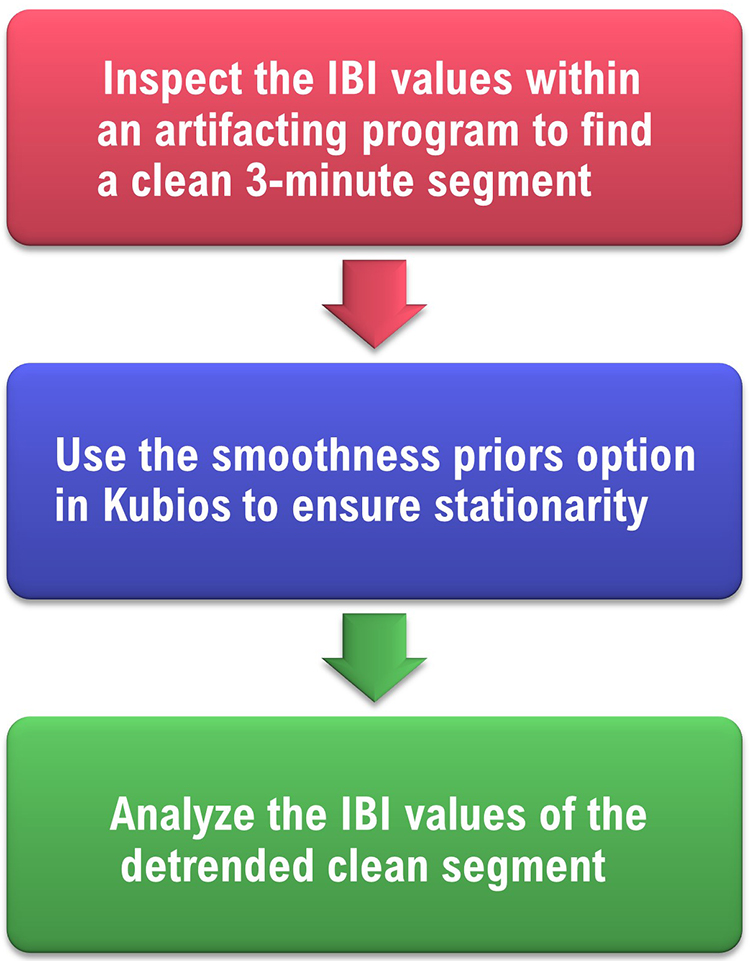
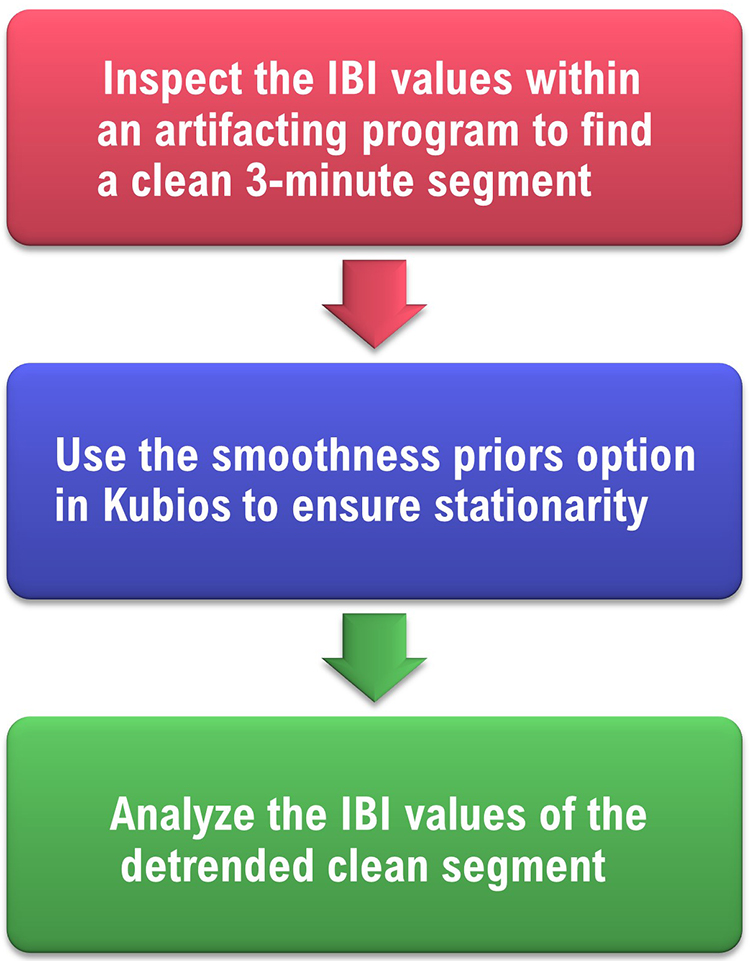
Plan A: Segment Removal and Detrending
When an epoch is at least 6 minutes long, and the artifact occurs in the first or last 3 minutes, you can analyze the clean 3-minute segment. The clean segment contains a set of interbeat interval (IBIs) values measured over an epoch and resembles an Excel column. We call this set of millisecond values a
time series. For example, 818.3 refers to 818.3 milliseconds.
Trends
Often during long measurement periods, there is a gradual change in the mean or variance of these IBIs, called a
trend.

Trends can violate an underlying stationarity assumption when measuring HRV time-domain, frequency-domain, and nonlinear values.
Stationarity means that the statistical properties of the IBI values (e.g., mean and standard deviation) do not change over time.
Acceptable and weak stationarity are illustrated below in graphics © Kubios Oy.
Caption: Acceptable Stationarity.
Caption: Weak Stationarity.
Detrending
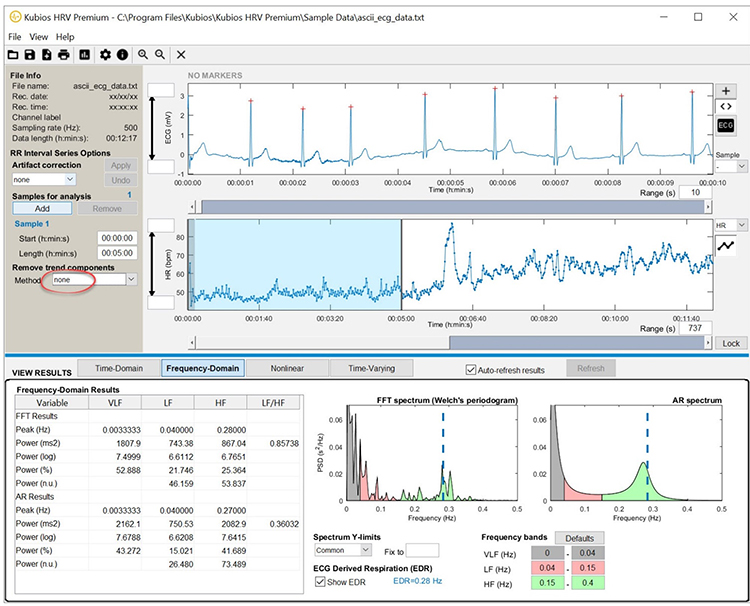
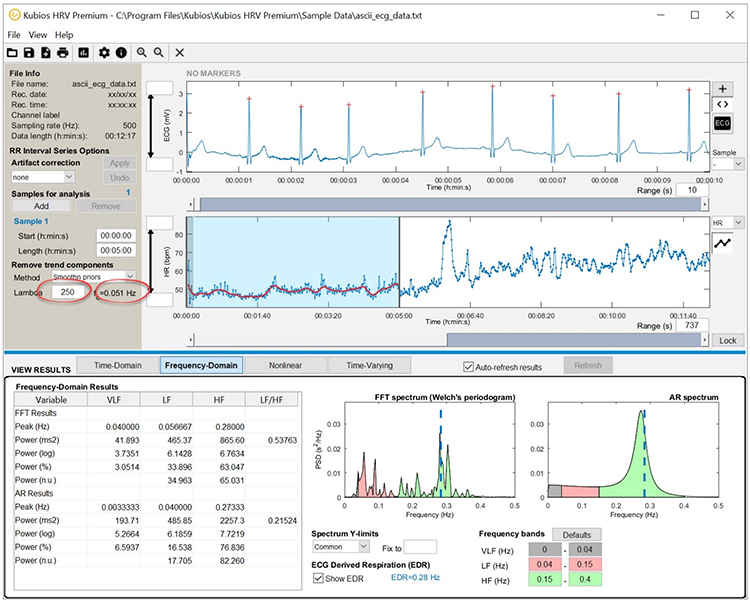
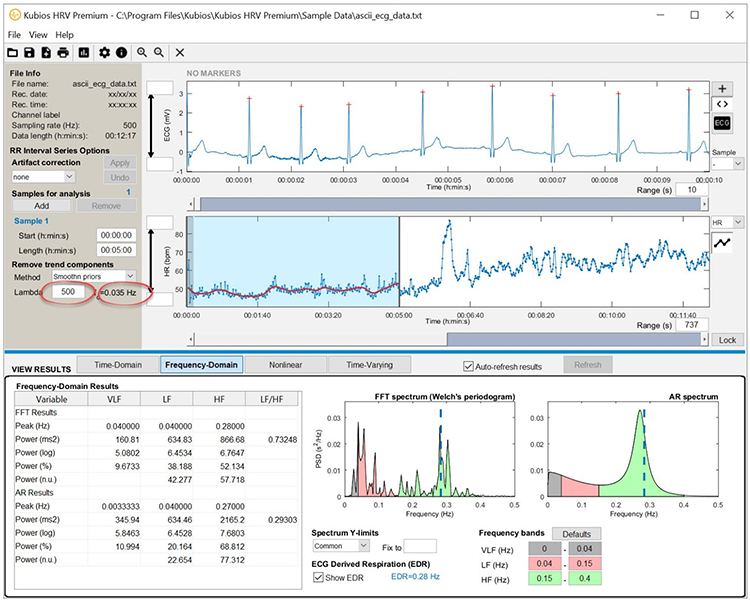
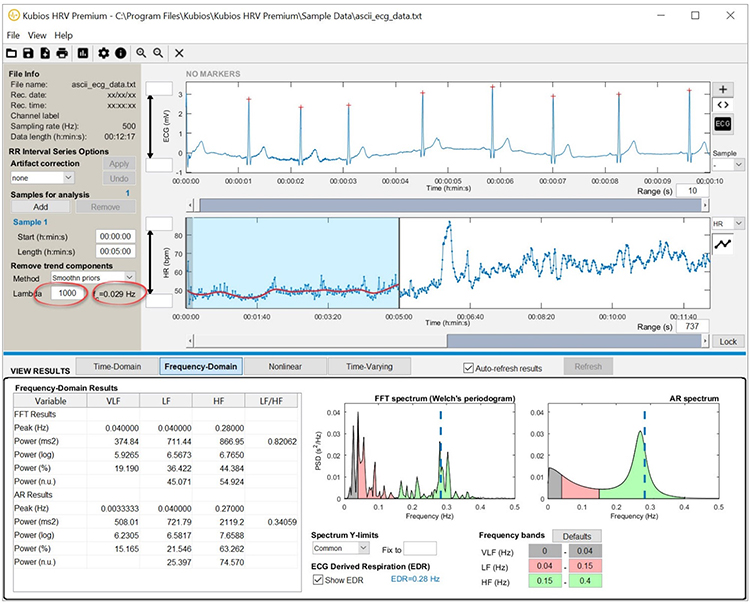
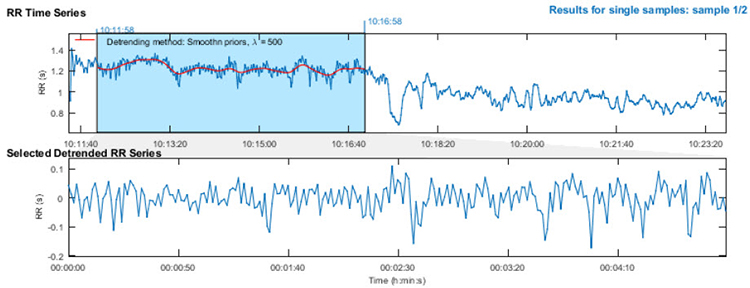
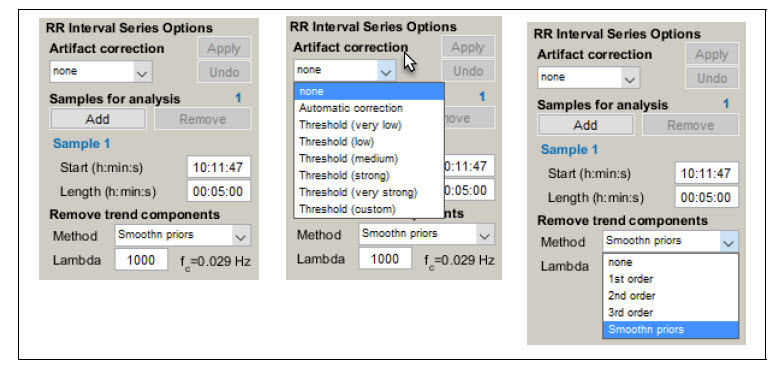
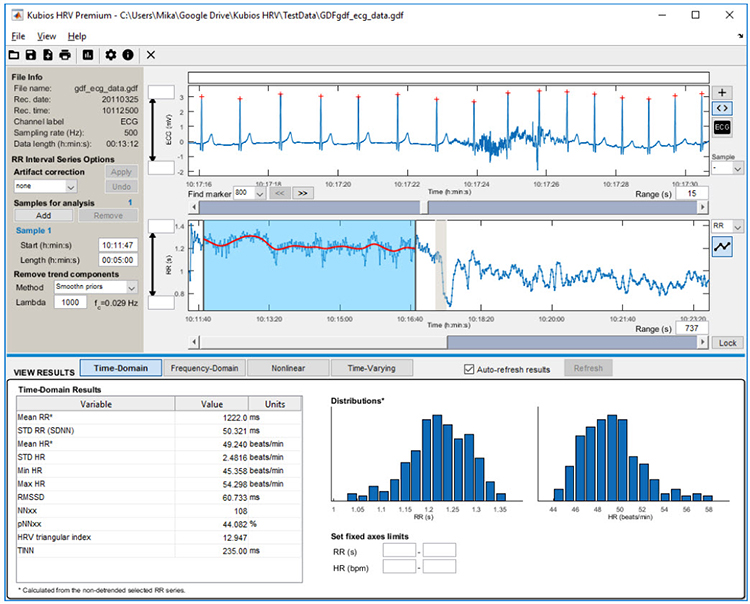
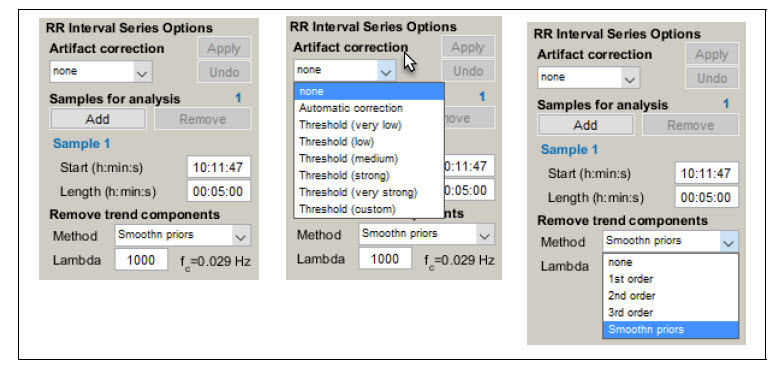
Detrending is the mathematical removal of a trend from a series. It is often used to ensure stationarity. Kubios provides a
smoothness priors function to remove the trend components from a time series. The smoothness priors function allows you to select the smoothness of the removed trend by manually entering a
lambda value. Lambda is the smoothing factor, and Kubios displays the corresponding cutoff frequency beside the lambda value you enter.
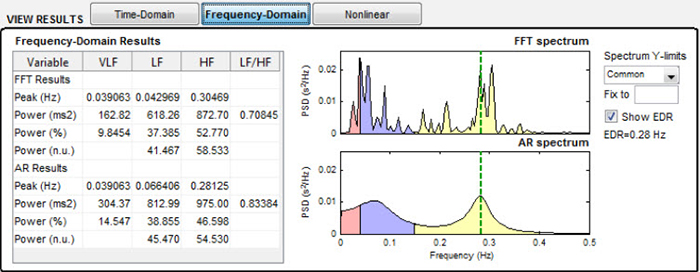
Increasing lambda values remove smoother (less jagged) trends. To preserve LF variability, you want the cutoff frequency to fall below 0.04 Hz. Exercise great caution in selecting lambda values so that you do not remove too much good data (Lehrer, 2018b).
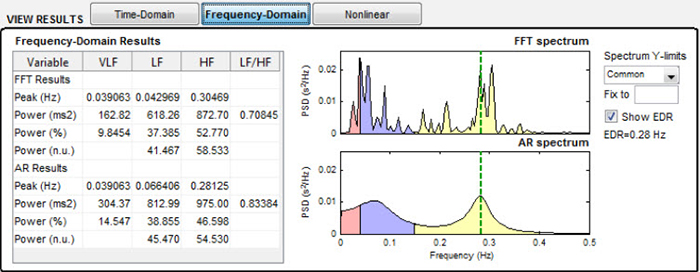
See how your lambda value affects the FFT spectrum (Tarvainen & Niskanen, 2020). The next graphics show no smoothing and increasingly higher lambda values of 250, 500, and 1000. All lambda values markedly reduce VLF power (0-0.04 Hz) and may also lower LF power (0.04-0.15 Hz).
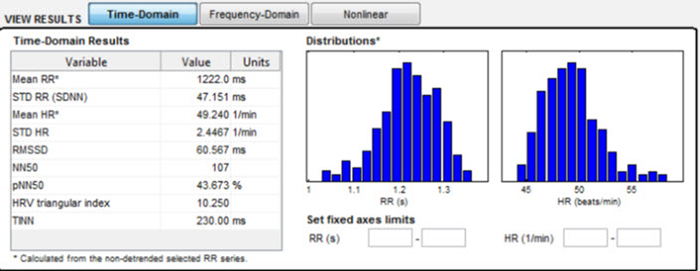
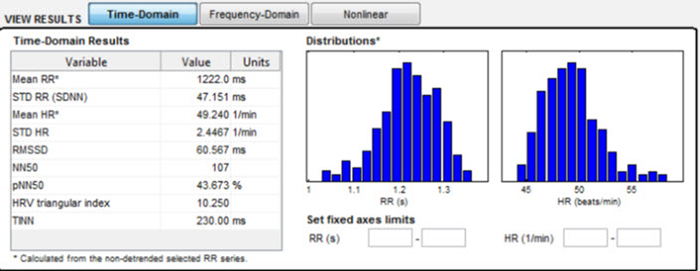
After detrending the IBI values, use the software to calculate the clean segment's time and frequency domain values.
Summary of Plan A
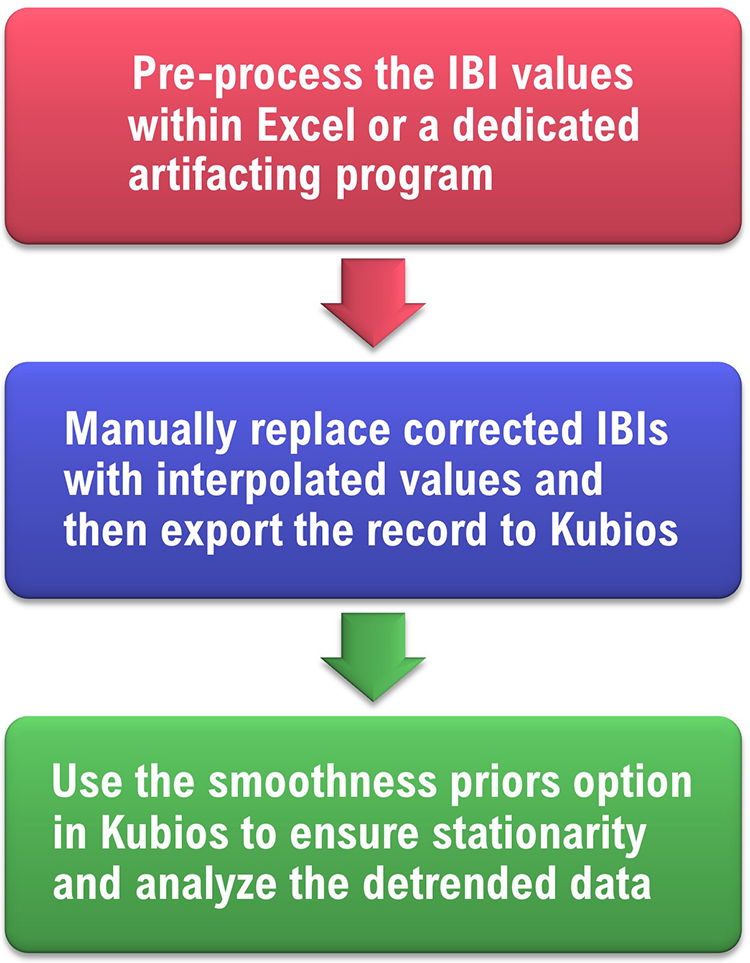
Plan B: Manual Correction and Detrending
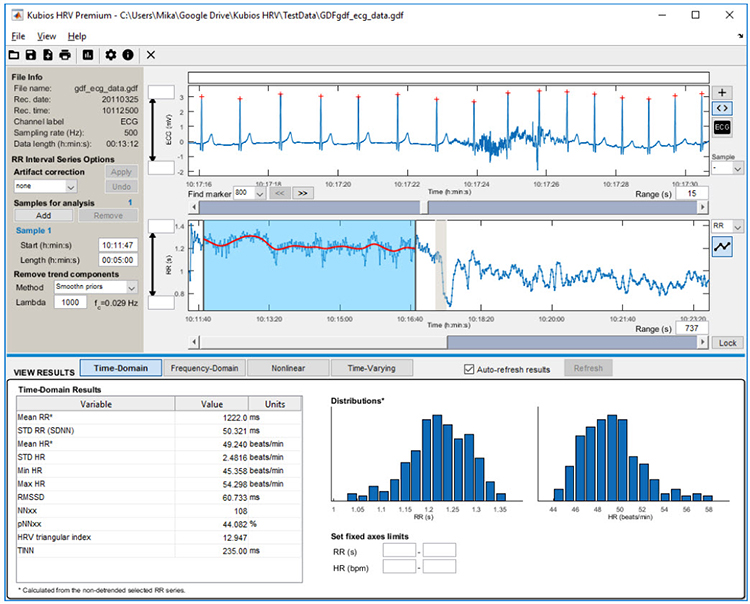
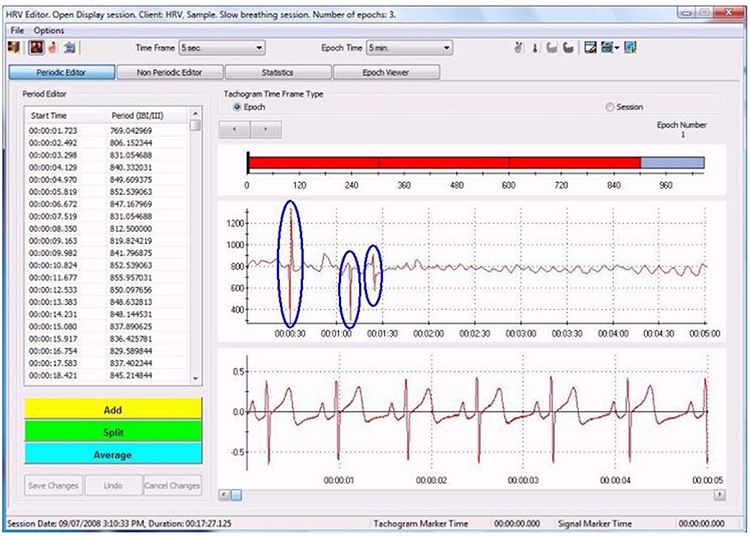
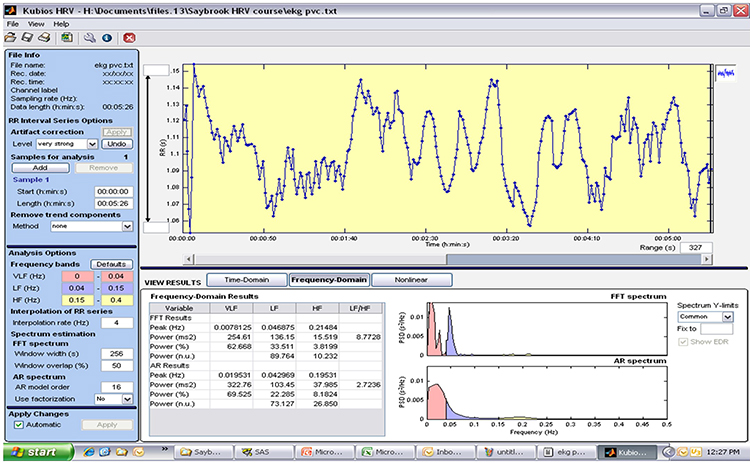
Manual correction and detrending is the best approach where you canít find a clean 5-minute or longer segment, and fewer than 5% of all beats are corrupted. Pre-process your data using Excel or a dedicated HRV analysis program like Thought Technology’s CardioPro ®.
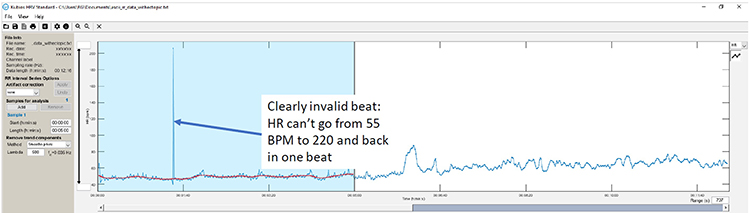
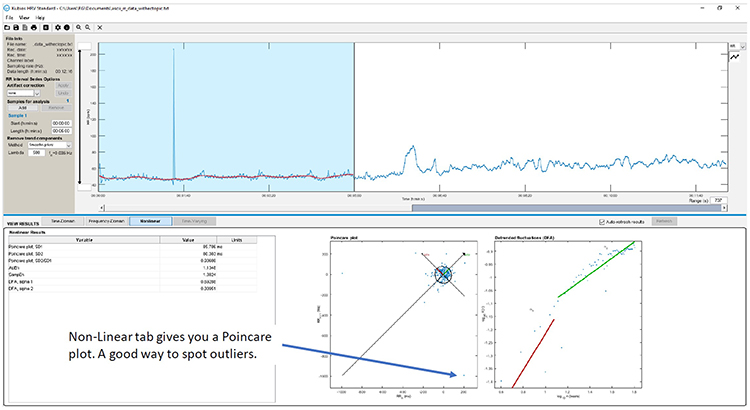
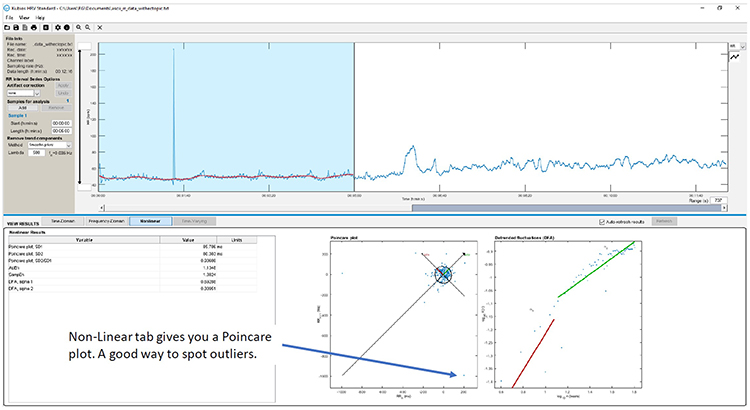
Kubiosí Time-Domain tab heart rate plot can help you visualize invalid beats (Gevirtz, 2018).
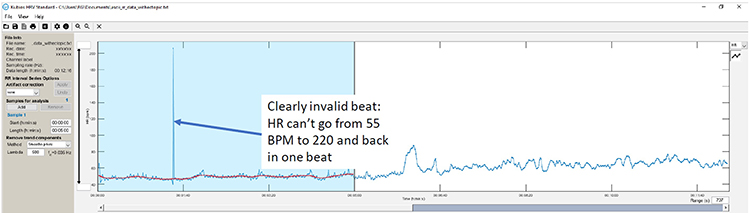
Kubiosí Non-Linear tab provides a Poincarť plot to help identify false beats (Gevirtz, 2018).
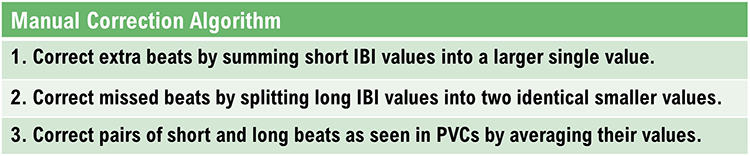
Correct extra beats and missed beats manually. Adjacent SEMG activity or ectopic beats produce extra beats that appear as very short IBIs.
Graphic © Kubios Oy.
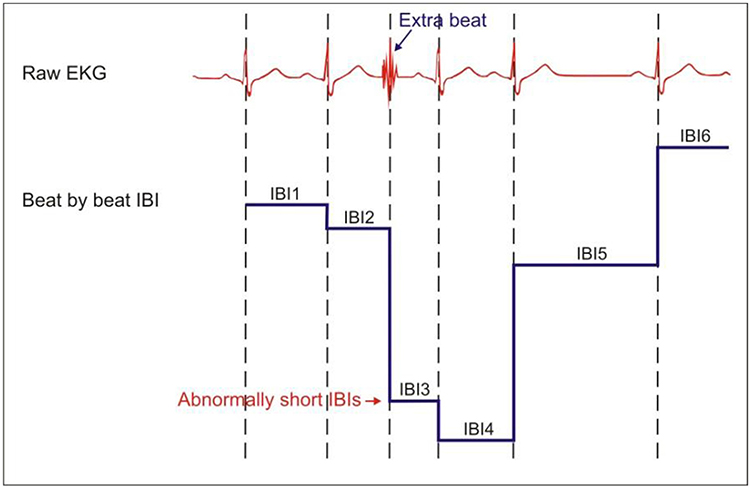
Caption: Extra beats shorten IBIs.
When the pulse wave (BVP) peak or the R-spike (ECG) amplitude are too low for recognition by software, this may result in missed beats that appear as prolonged IBIs. Graphic © Kubios Oy.
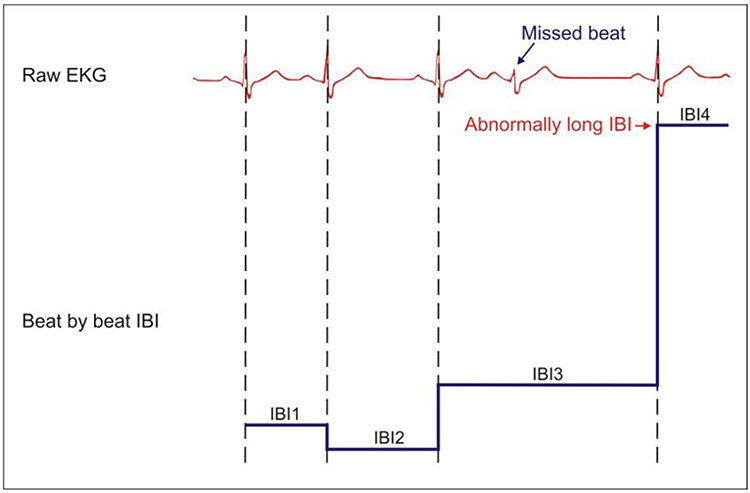
Caption: Missed beats lengthen IBIs.
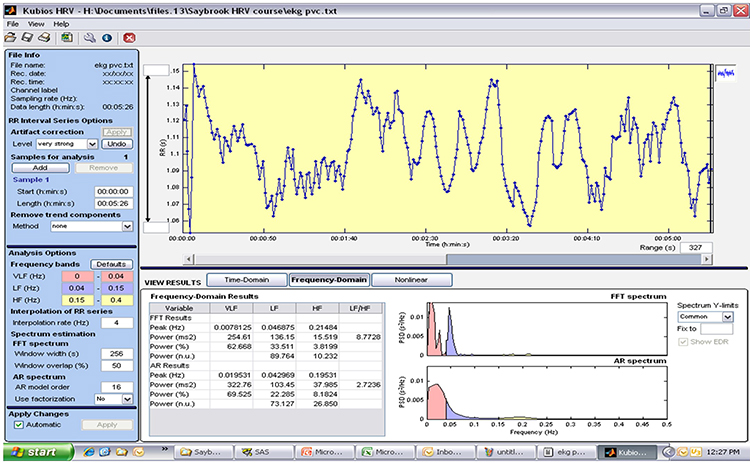
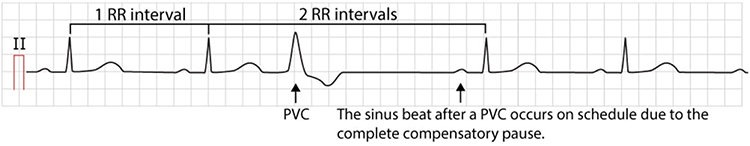
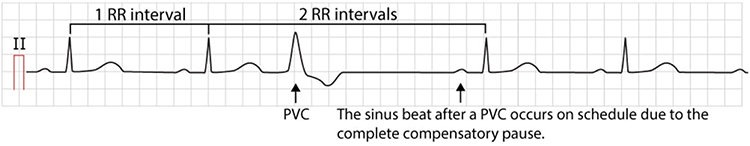
PVCs can result in an extra heartbeat followed by a full compensatory pause.
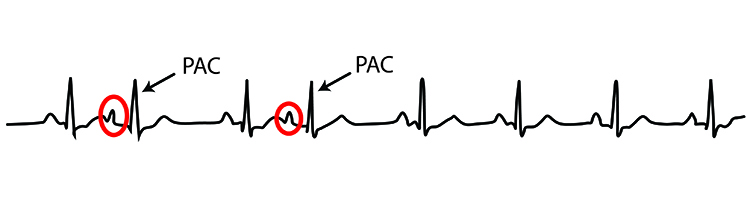
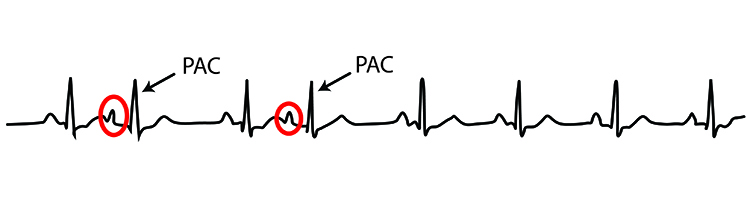
An ectopic pacemaker initiates
premature atrial complexes (PACs) in the atria. Since PACs involve an extra beat without a compensatory beat, there is no easy way to remove them through manual artifacting.
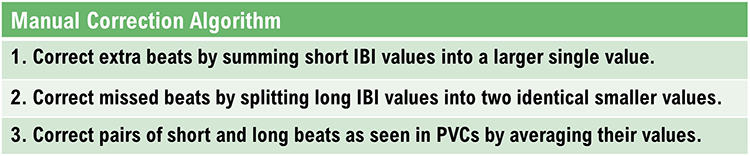
In the graphic below, you can see the Add, Split, and Average options at the bottom left of CardioProís data editing window. Highlight the abnormal beats (circled in blue) in the data window and select the appropriate correction.
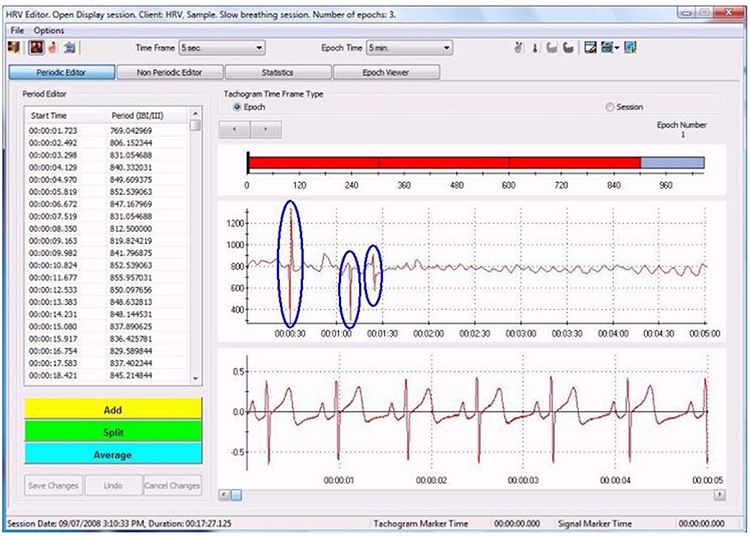
At the current state of the art, manual editing is usually superior to automated editing.
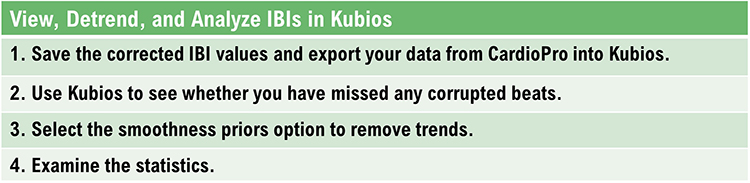
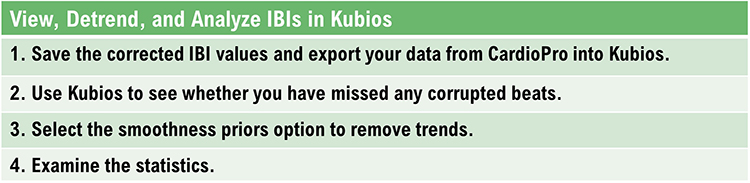
Summary of Plan B
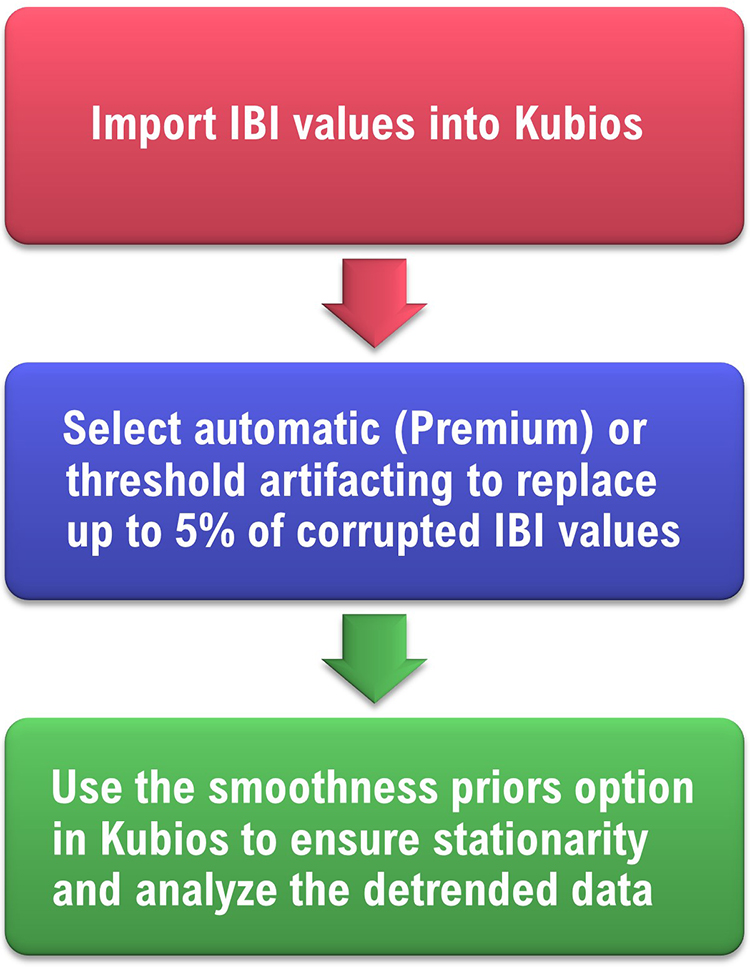
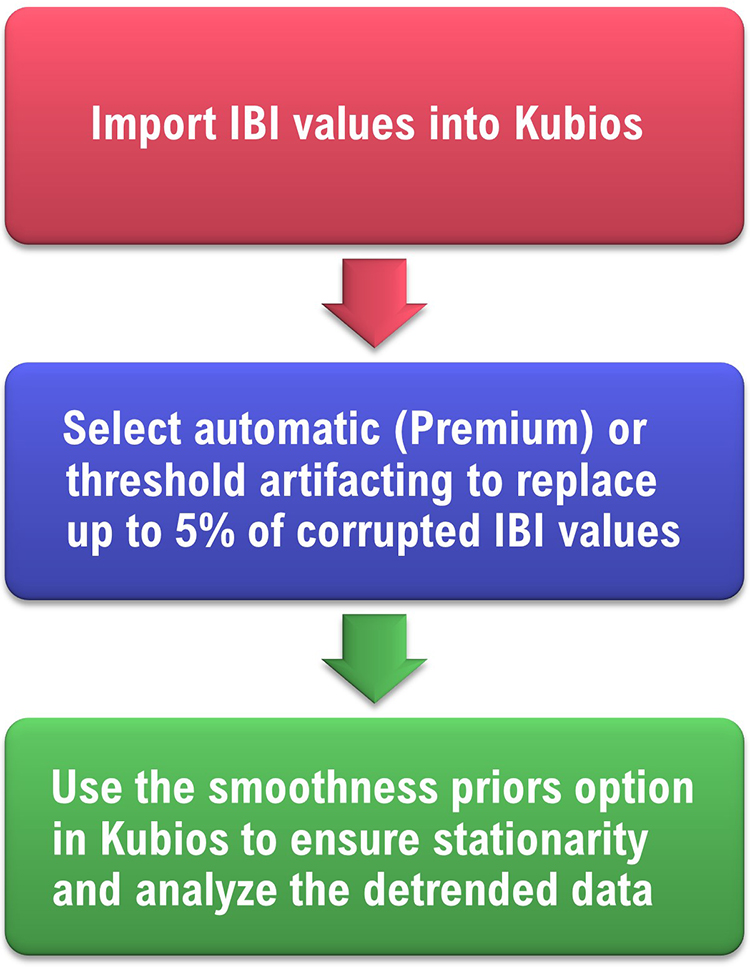
Plan C: Automated Correction
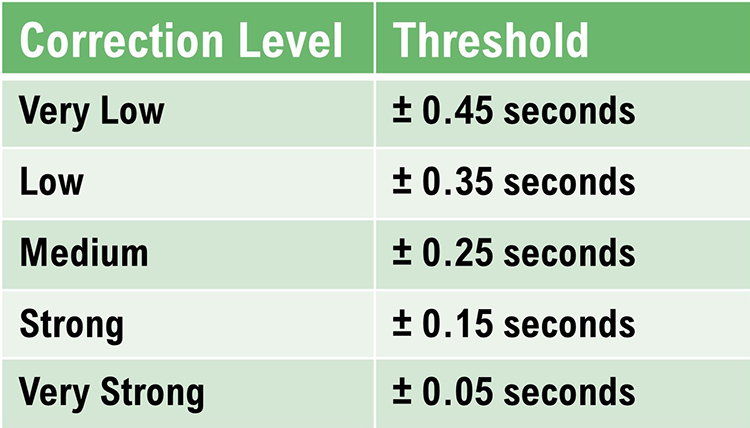
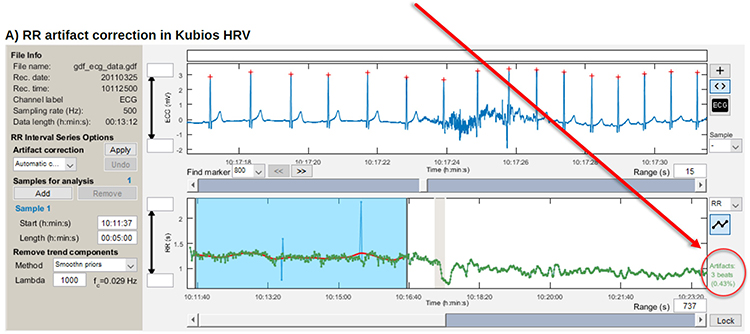
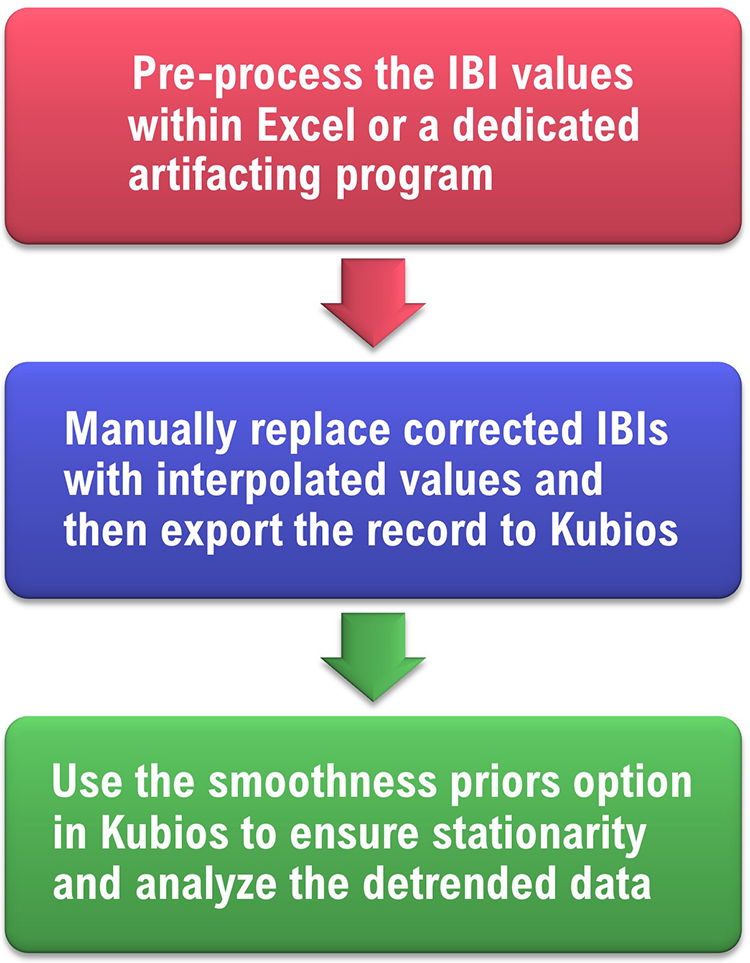
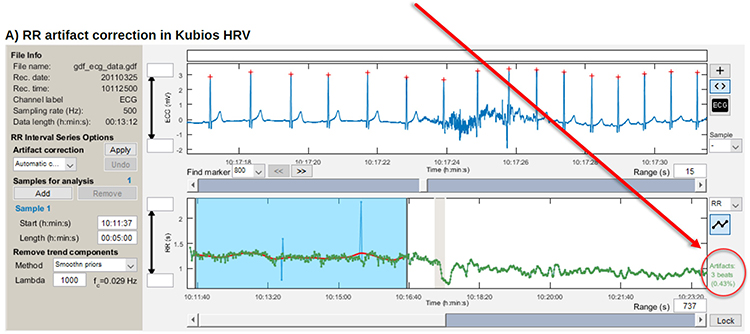
Kubios provides five preselected correction levels and a user-defined level.
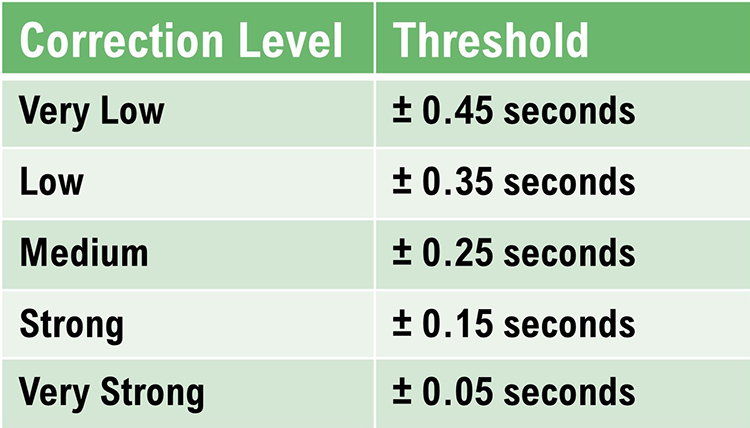
After selecting a correction level, you can see whether it adequately identifies invalid IBIs. When you are satisfied with a levelís sensitivity, you may press the Apply button to replace corrupted IBIs with interpolated ones.
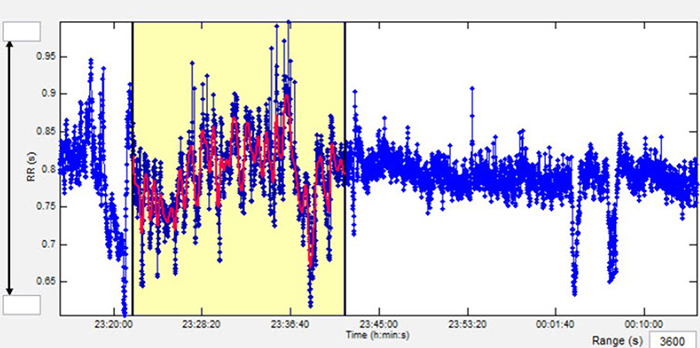
Kubios shows new (red) values superimposed over the original (blue) values.
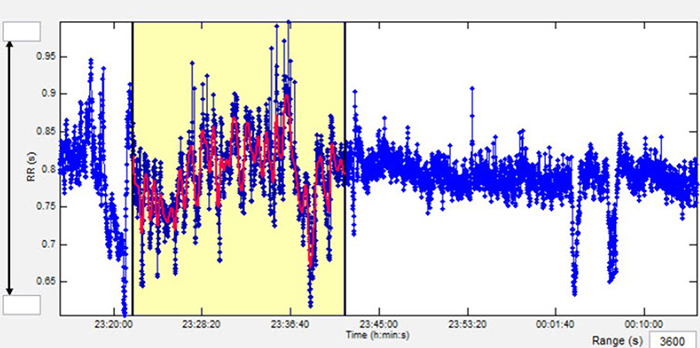
Kubios shows the number of corrected beats and its percentage of the total.
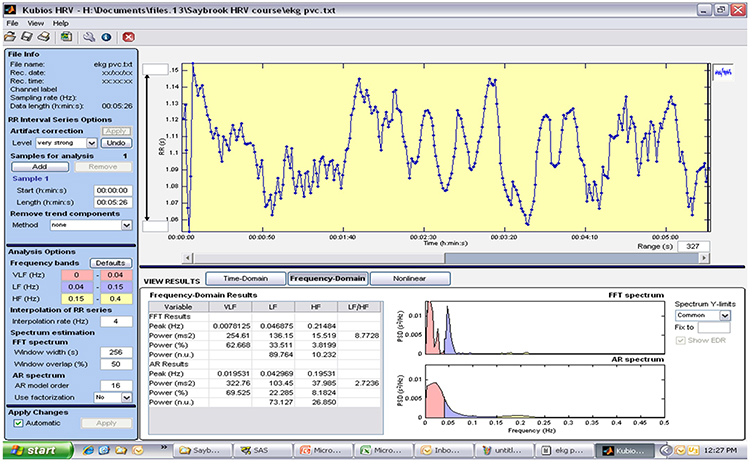
The table below shows HRV metrics without and with automatic artifact correction.
Compare RMSSD values: 136.38 ms without correction and 57.79 ms with correction.

Next, click the Read More button for medium-threshold and very-high-threshold artifact correction using Kubios courtesy of Paul Lehrer (2018a).
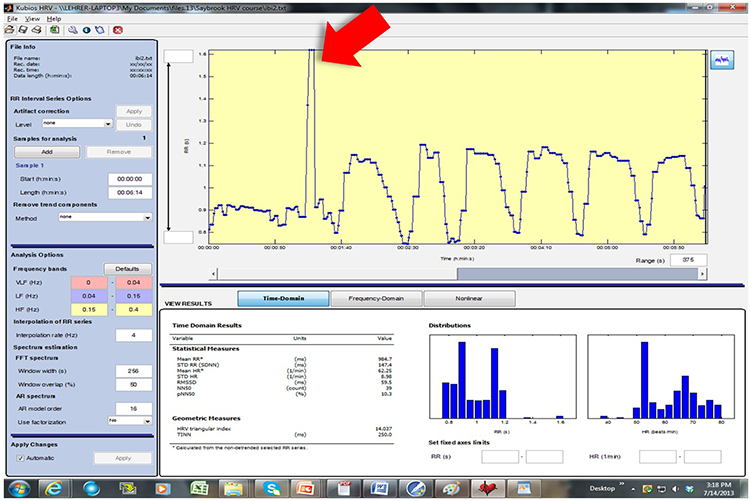
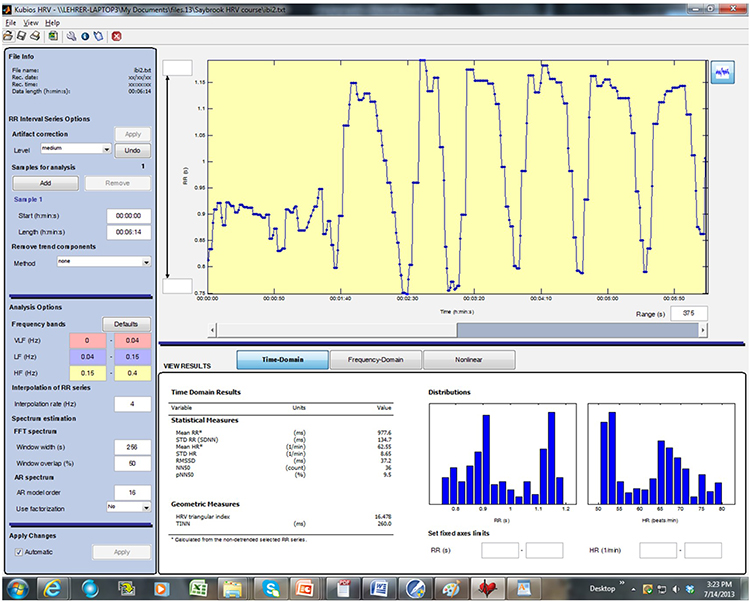
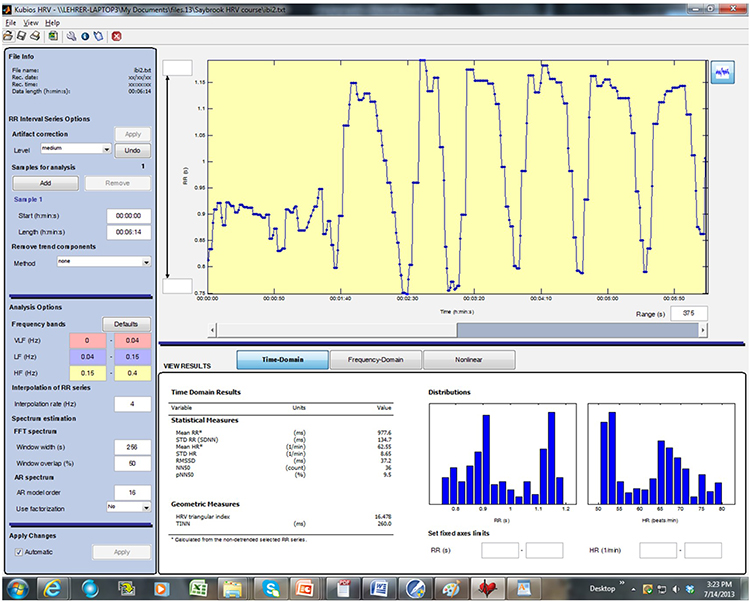
Kubios data with artifact around 00:01:00 probably due to missed low-amplitude R-spikes The vertical axis is the IBI in milliseconds. The IBI is over 1600 ms.
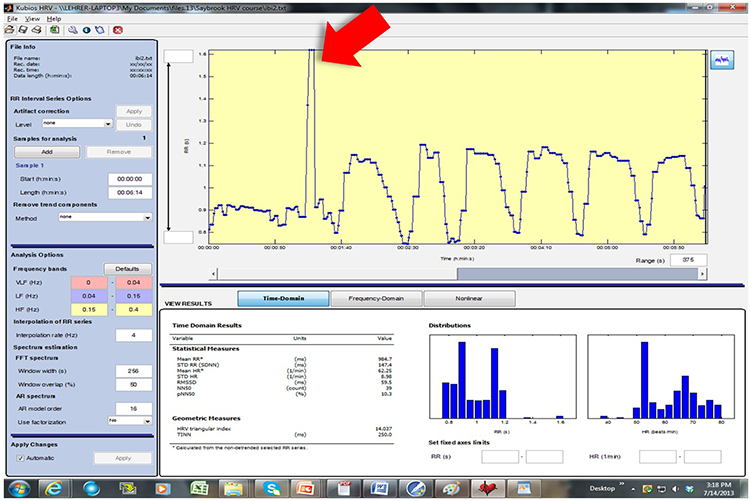
This graphic illustrates medium-threshold artifact correction. Artifact = blue and corrected IBIs = green.
The vertical axis is the IBI in milliseconds.
This graphic shows saved data following artifact correction. The vertical axis is the IBI in milliseconds.
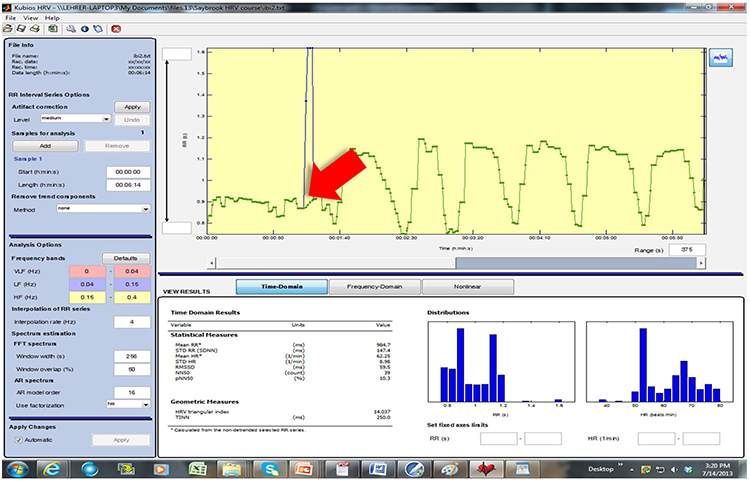
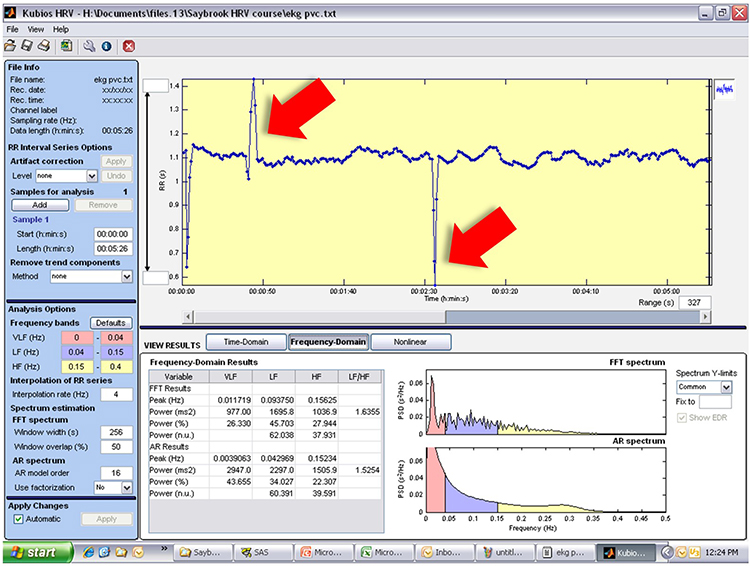
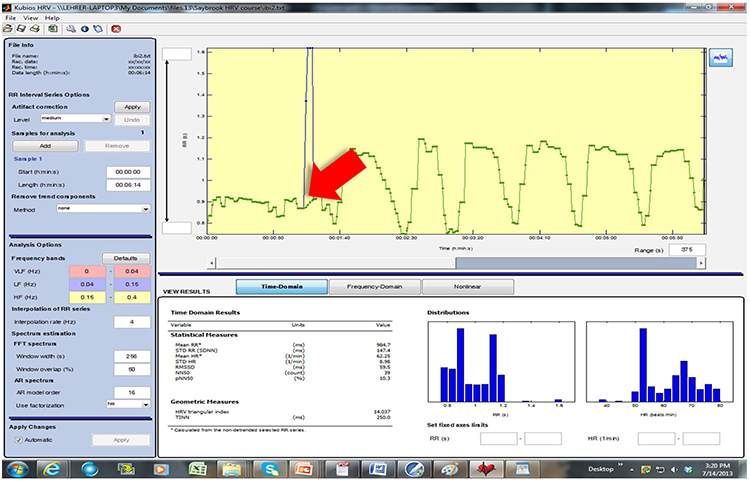
This graphic shows Kubios data with artifacts around 00:00:50 and 00:02:30. The vertical axis is the IBI in milliseconds.
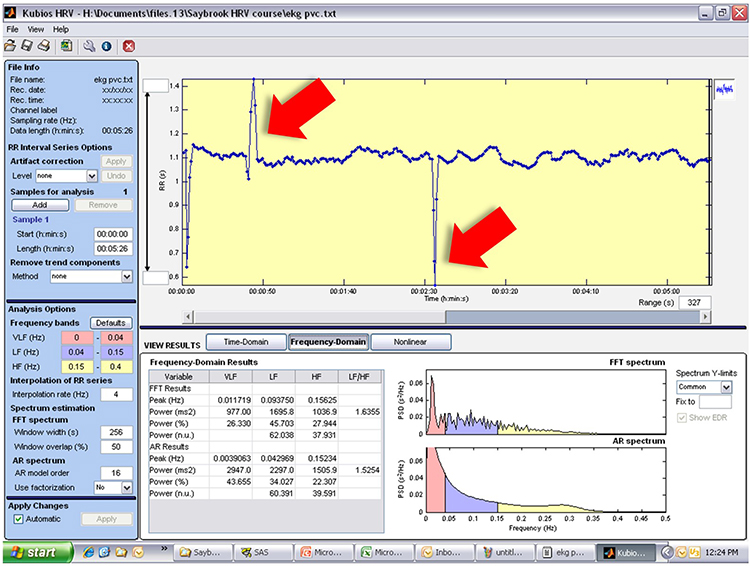
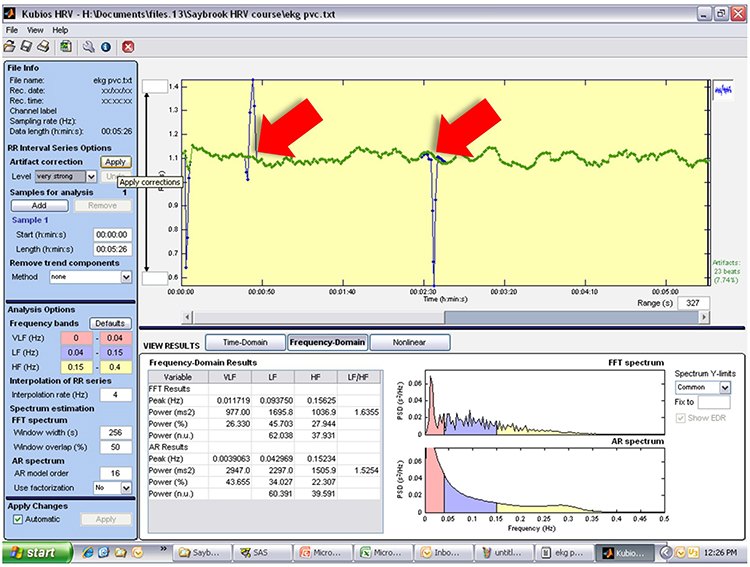
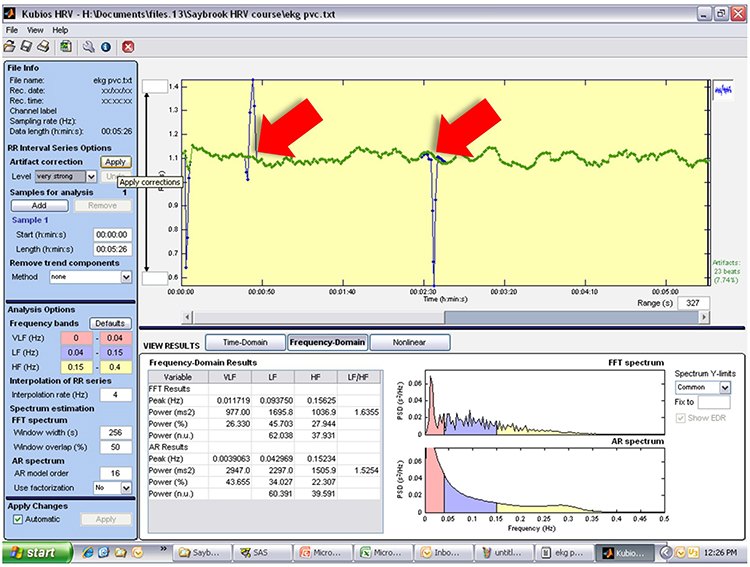
This graphic shows
very-strong-threshold artifact correction. The vertical axis is the IBI in milliseconds. Artifact = blue and corrected IBIs = green.
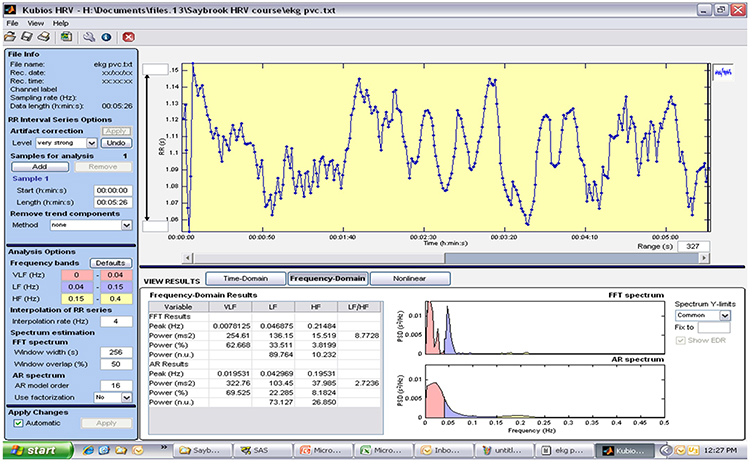
This graphic shows saved data following artifact correction. Next, select the smoothness priors option to remove trends.
Summary of Plan C
 A clinician calculated LF and HF power after deleting sections of a 5-minute recording period contaminated by artifacts. Which error did they commit?
A clinician calculated LF and HF power after deleting sections of a 5-minute recording period contaminated by artifacts. Which error did they commit?
The "hack and stitch" strategy distorts the temporal relationship between the IBIs and yields invalid frequency-domain measurements. Instead, they should have split excessively long IBIs, added short IBIs together, and averaged pairs of long and short IBIs.
A Practical Perspective
Artifacting is as vital in HRV biofeedback as it is in neurofeedback. While the high-level processing of interbeat interval data described in this unit is required to publish research, less intensive data analysis is sufficient for HRV biofeedback training.
Clinicians can limit their review of session data to pre- and post-baselines. They may not need to detrend 5-minute data sets and may be able to skip artifacting entirely if they can find 3 consecutive minutes of clean data. If artifacts have corrupted all 5 minutes of data, they can examine the adequacy of automatic artifacting within their analysis software and use manual artifacting as a last resort. Artifacting skills can be readily mastered through the guidance of an experienced mentor. Contact the Biofeedback Certification International Alliance (BCIA) or your vendor for mentor recommendations.

Glossary
artifacts: measurement errors in calculating the interbeat interval.
artifacting: the process of removing or replacing false values found within a data
record.
detrending: the mathematical removal of a trend from a time series to ensure stationarity.
ectopic beats: beats initiated outside of the S-A node that produce consecutive IBI values that are abnormally long and short.
epoch: a data collection period.
extra beats: ECG artifacts that shorten the IBI when signal distortion causes the software to detect nonexistent beats.
heart rate variability (HRV): the beat-to-beat changes in heart rate that include changes in the RR intervals between consecutive heartbeats.
interbeat interval (IBI): the time interval between the peaks of successive R-spikes (initial upward deflections in the QRS complex). The IBI is also called the NN (normal-to-normal) interval.
lambda: the parameter that specifies the smoothness of the removed trend in the smoothness priors method.
missed beats: an ECG artifact that lengthens the IBI when signal distortion causes the software to overlook a beat and use the next good beat.
premature atrial complexes (PACs): ectopic beats originating within a pacemaker in the atria.
smoothness priors method: a mathematical method for removing trends of a specific smoothness from a time series.
stationarity: the assumption that the statistical properties of a series of values (e.g., mean and standard deviation) do not change over time.
time series: a set of values (IBIs) measured over time.
trend: a gradual change in a statistical property (mean or standard deviation) of a time series.
Test Yourself
Click on the ClassMarker logo to take 10-question tests over this unit without an exam password.

REVIEW FLASHCARDS ON QUIZLET
Click on the Quizlet logo to review our chapter flashcards.

Visit the BioSource Software Website
BCIA offers two HRV Biofeedback Certification paths: Biofeedback and Neurofeedback.
For Biofeedback, BioSource Software offers
Human Physiology to satisfy BCIA's Human Anatomy & Physiology requirement. For Neurofeedback, BioSource provides
Physiological Psychology to satisfy BCIA's Physiological Psychology requirement.
BCIA has accredited each course, and they combine affordable pricing ($150) with industry-leading content.

Assignment
Now that you have completed this module, review the missed beat and extra beat graphics and see whether you can identify abnormally long and short IBIs. Based on this module, how might you improve your artifacting.
Acknowledgment
This article draws heavily on graphics published in Didier Combatalade’s
Basics of Heart Rate Variability Applied to Psychophysiology, published by Thought Technology Ltd., and Tarvainen and Niskanen's
Kubios HRV User's Guide. A special thanks to Dick Gevirtz for sharing Alliant University’s artifacting protocol. Dick is a gifted clinician, educator, and researcher.

References
Aldini, M. (2016). Issues in heart rate variability (HRV) analysis: Motion artifacts & ectopic beats. Blog post: https://www.hrv4training.com/blog/issues-in-heart-rate-variability-hrv-analysis-motion-artifacts-ectopic-beats.
Berntson, G. G., Bigger, J. T., Jr., Eckberg, D. L., Grossman, P., Kaufmann, P. G., Malik, M., Nagaraja, H. N., Porges, S. W., Saul, J. P., Stone, P. H., & Van Der Molen, M. W. (1997).
Heart rate variability: Origins, methods, and interpretive caveats.
Psychophysiology, 34, 623-648.
Berntson, G. G., & Stowell, J. R. (1998). ECG artifacts and heart period variability: Don’t miss a beat!
Psychophysiology, 35, 127-132. PMID: 9499713
Cherif, S., Pastor, D., Nguyen, Q.-T., & L’Her, E. (2016). Detection of artifacts on photoplethysmography signals using random distortion testing. 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). https://doi.org/10.1109/EMBC.2016.7592148
Clinical EEG Interpretation (2018). Premature ventricular contractions (premature ventricular complex, premature ventricular beats. https://ecgwaves.com/premature-ventricular-contractions-complex-beats-ecg/
Combatalade, D. (2010).
Basics of heart rate variability applied to psychophysiology. Montreal, Canada: Thought Technology Ltd.
Combatalade, D. (2013).
CardioPro Infiniti: HRV analysis module for BioGraph Infiniti. Montreal, Canada:
Thought Technology Ltd.
Elgendi, M. (2012). On the analysis of fingertip photoplethysmogram signals.
Current Cardiology Reviews, 8, 14‐25. https://dx.doi.org/10.2174%2F157340312801215782
Gevirtz, R. (2018). Personal communication about artifacting.
Kuusela, K. (2013). Methodological aspects of heart rate variability analysis. In M. V. Kamath, M. A. Watanabe, & A. R. M. Upton (Eds.).
Heart rate variability (HRV) signal analysis. Boca Raton, FL: CRC Press.
Langner, P. H. Jr., & Geselowitz, D. B. (1960). Characteristics of the frequency spectrum in the normal electrocardiogram and in subjects following myocardial infarction.
Circ Res, 8, 577-584.
Lehrer, P. (2018a). Heart rate, interbeat interval, and the electrocardiogram (shared presentation).
Lehrer, P. (2018b). Personal communication about artifacting.
Nederend, I., Jongbloed, M. R. M., de Geus, E. J. C., Blom, N. A., & ten Harkel, A. D. J. (2016). Postnatal cardiac autonomic nervous control in pediatric congenital heart disease.
J Cardiovasc Dev Dis, 3(2) 16. https://doi.org/10.3390/jcdd3020016
Peper, E., & Lin, I.-M. (2009). Keep cell phones and PDAs away from EMG sensors and the human body to prevent electromagnetic interference artifacts and cancer.
Biofeedback, 37(2), 114-116. https://doi.org/10.5298/1081-5937-37.3.114
Peper, E., Shaffer, F., & Lin, I-M. (2010). Garbage In; Garbage out—Identify blood volume pulse (BVP) artifacts before analyzing and interpreting BVP, blood volume pulse amplitude, and heart rate/respiratory sinus arrhythmia data.
Biofeedback, 38(1), 19-23. https://doi.org/10.5298/1081-5937-38.1.19
Shaffer, F., & Combatalade, D. C. (2013).
Don't add or miss a beat: A guide to cleaner heart rate variability recordings.
Biofeedback, 41(3),
121-130.
Stern, R. M., Ray, W. J., & Quigley, K. S. (2001).
Psychophysiological recording (2nd ed.). Oxford University Press.
Tarvainen, M. P., & Niskanen, J.-P. (2020).
Kubios HRV version 3.2 user's guide. University of Finland.
Task Force of the European Society of Cardiology and the North American
Society of Pacing and Electrophysiology (1996).
Heart rate variability: Standards of measurement, physiological interpretation, and clinical use.
Circulation, 93, 1043-1065. PMID: 8598068