We develop
specific immunity after
birth through exposure to microorganisms and vaccinations, and it
employs an
antigen-antibody reaction
to protect us against specific microorganisms and their toxins.
Antigens are foreign molecules (proteins or polysaccharides) that
stimulate antibody production.
Antibodies
are cellular proteins that combine with antigens to neutralize them.
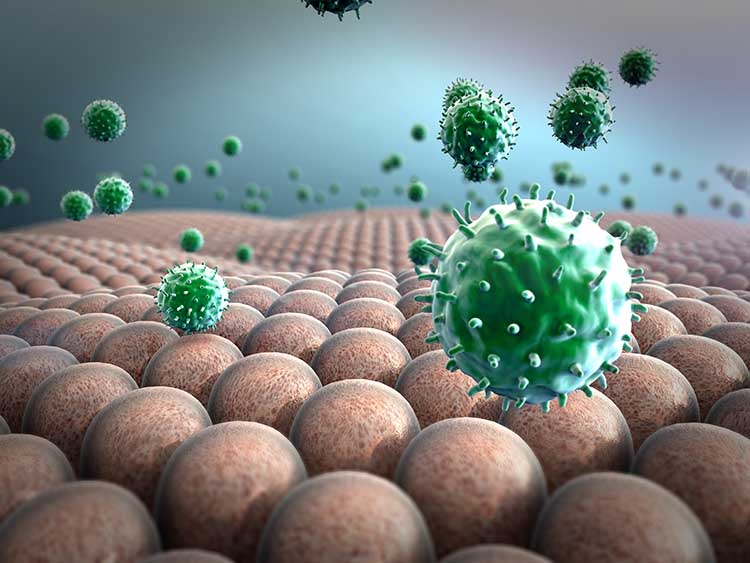
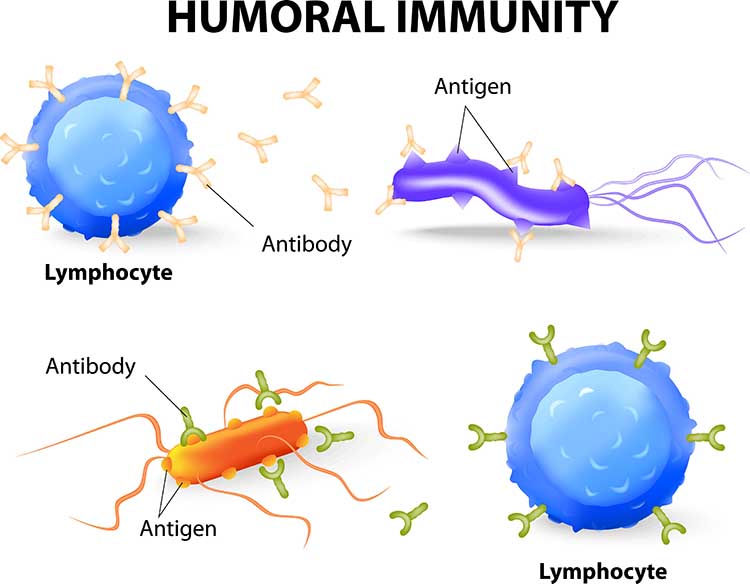
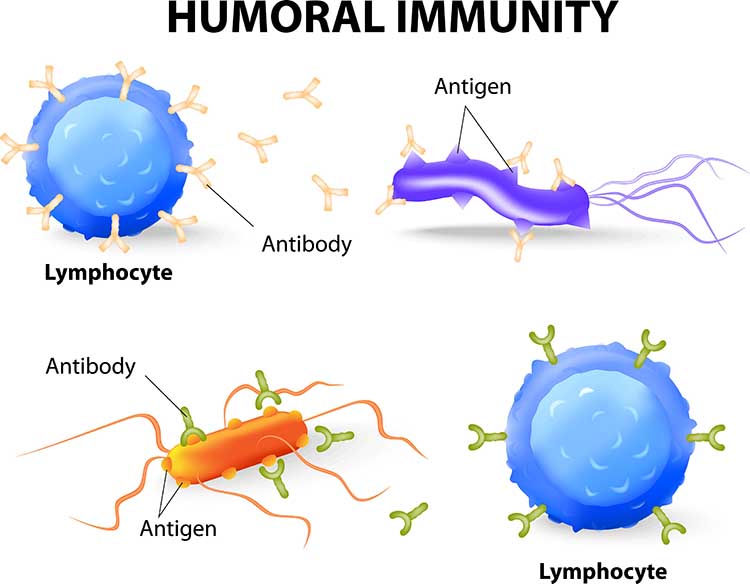
Humoral and cell-mediated immunity are two types of specific immune
responses. In
humoral immunity,
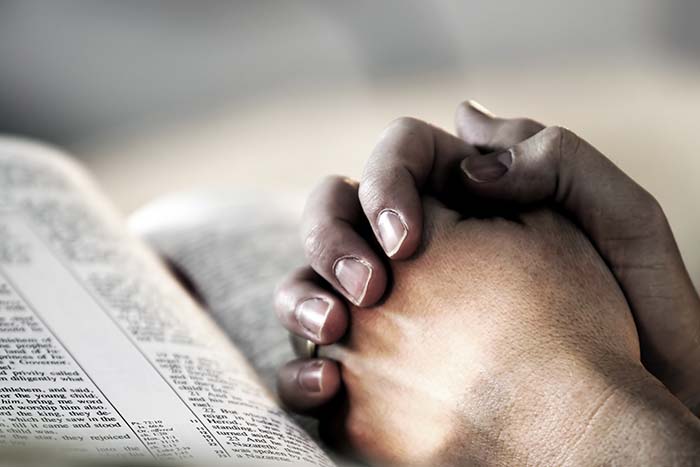
B lymphocytes rapidly produce antibodies that counter bacteria into the blood, neutralize
toxins, and prevent reinfection by viruses. The illustration below shows lymphocytes (white) attacking bacteria. Graphic © dreamerb/Shutterstock.com.

Activated B cells
differentiate into
plasma cells,
which secrete antibodies (immunoglobulins), and
memory B cells, which are transformed into
antigen-specific plasma cells when they reencounter the original
antigen. Humoral immunity is most effective in countering bacterial
infections and preventing new viral infections. The illustration below shows lymphocytes (white) attacking bacteria. Graphic © Designua/Shutterstock.com.
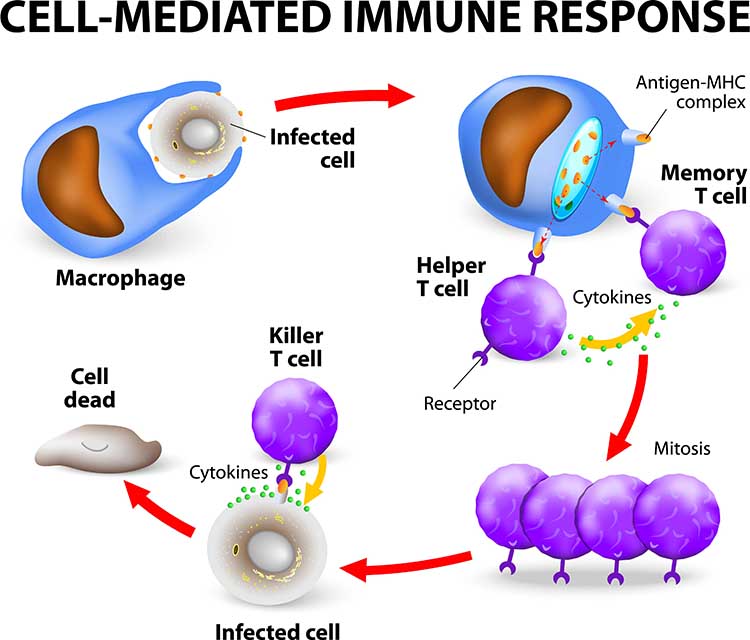
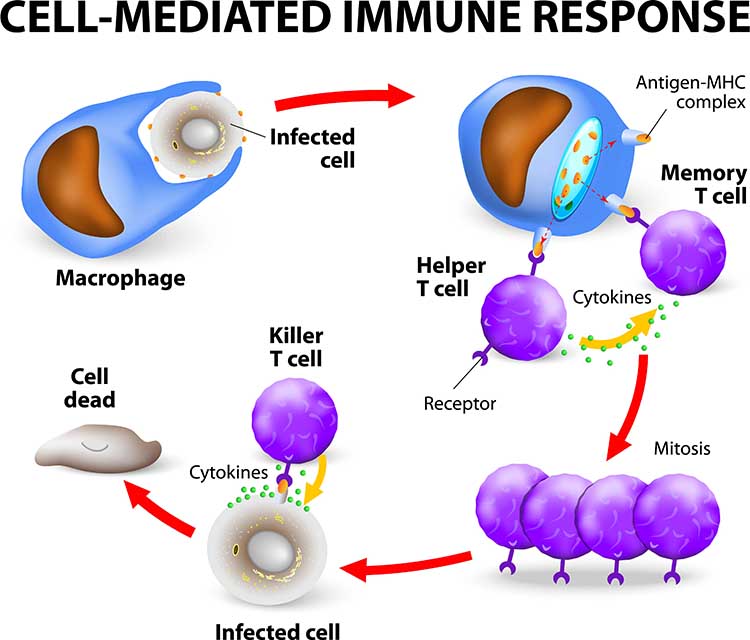
Cell-mediated immunity provides a
slower cellular response that utilizes cytotoxic and helper T cells
from T lymphocytes provided by the thymus gland.
Cytotoxic T (TC)
cells release toxins to destroy specific virally infected
cells.
Helper T (TH)
cells release cytokines like interleukin-2 to aid T
C and B cells' action and macrophages. T
H cell
cytokines can also suppress immune responses. Cell-mediated
immunity is most effective in controlling cancer, foreign tissue, fungal
and viral infections, and parasites.
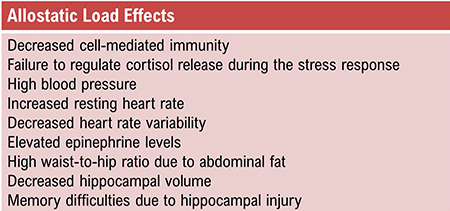
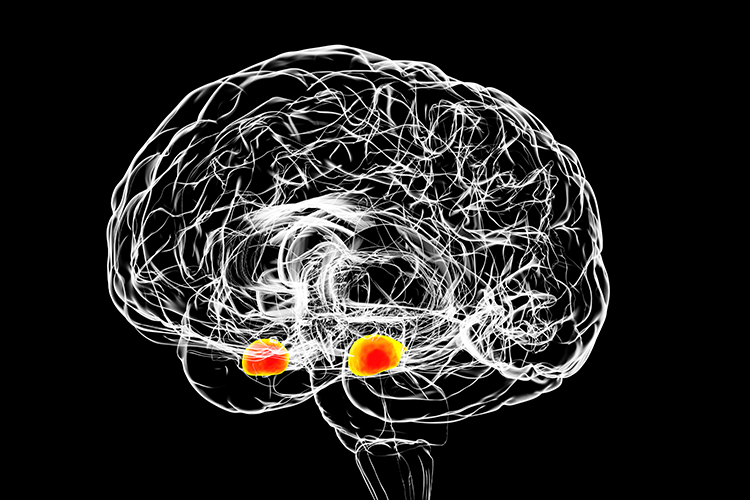
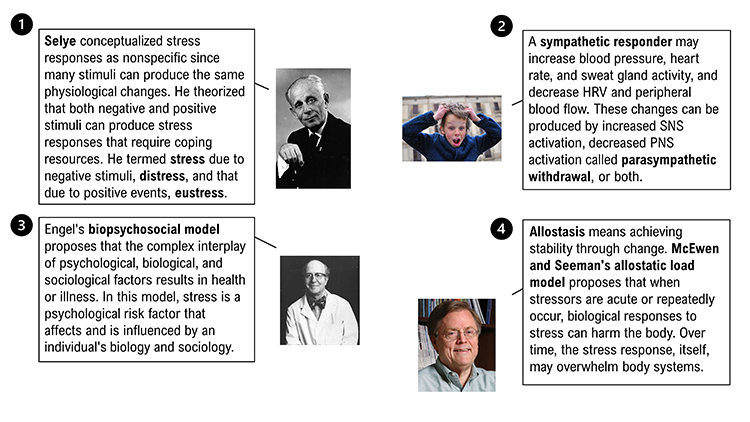
Two-Way Brain-Immune System Communication
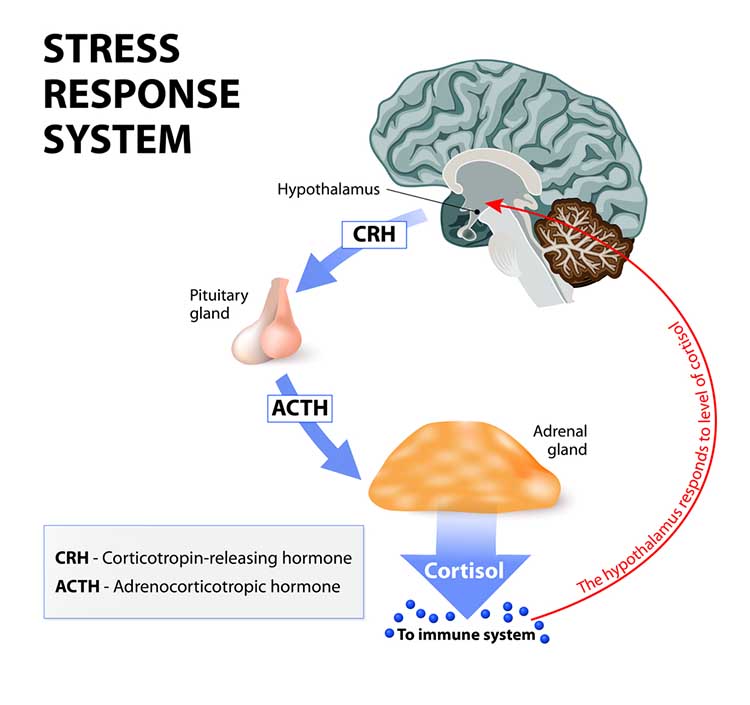
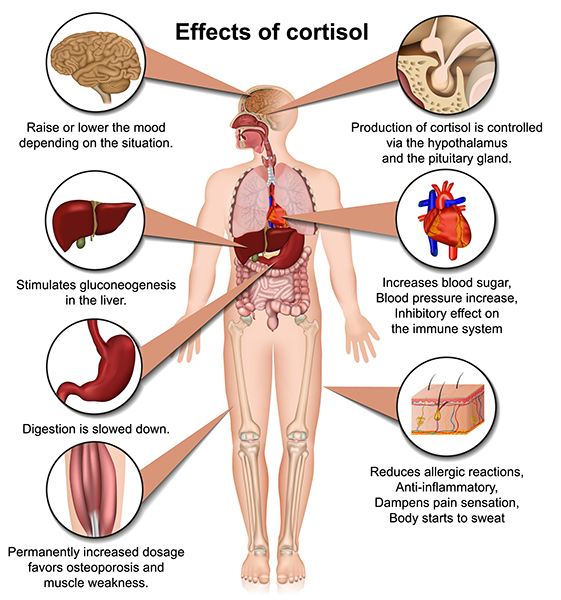
Nervous and immune system communication is bidirectional. From the nervous system side, the adrenal cortical release of glucocorticoids suppresses immunity, including cell-mediated mechanisms like phagocytosis. At the start of the COVID-19 pandemic, admitted patients with higher cortisol levels were more likely to die from this infection (Tan et al., 2020).
From the immune system side, increased proinflammatory cytokine release can signal the nervous system, resulting in feelings of depression, fatigue, loss of energy, and reduced pleasure (Anisman et al., 2005; Brannon et al., 2022; Dantzer et al., 2008). Acute and prolonged brain fog due to COVID-19 has been attributed to elevated cytokine levels (Theoharides et al., 2021). Graphic © Designua/Shutterstock.com.
Check out Professor Gillian Griffiths' video
Killer T Cell: The Cancer Assassin.
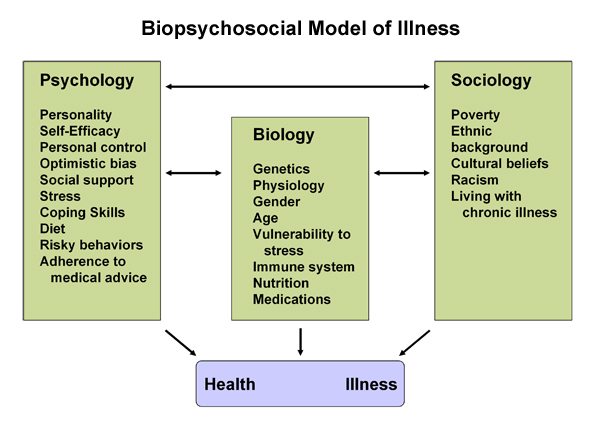
The Immune System Is Interconnected with the Nervous System
The classical model of the immune system is that it operates
independently of the nervous system and psychological processes.
However, researchers have demonstrated complex interactions among the nervous, endocrine, and immune systems, consistent with Green and Green's psychophysiological principle. Psychological
processes like expectancies (placebo effect) and learning (classical
conditioning) can affect all three systems, and the immune system can
affect psychological functioning (drowsiness from a fever).
Psychoneuroimmunology is a
multidisciplinary field that studies the interactions between behavior
and these three systems.
After Solomon and Moos (1964)
introduced the term psychoneuroimmunology in a journal article,
Ader and Cohen's (1975) demonstration of classical conditioning in a rat's
immune system helped
establish this field's scientific legitimacy.
Ader and Cohen trained
rats to associate a
conditioned stimulus
(a
saccharine and water solution)
with an
unconditioned stimulus (the
immunosuppressive drug cyclophosphamide). This resulted in a
conditioned response (CR) of immune
suppression, which resulted in rat fatalities. Following conditioning,
rats who drank only sweetened water (CS) died due to
conditioned immunosuppression.
Successful replication of these findings helped overcome resistance to
the controversial view that the nervous and immune systems interact.
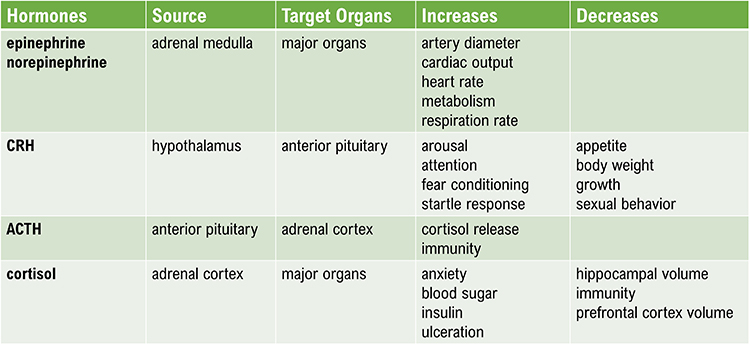
The mechanisms underlying these complex interactions include
HPA axis hormones (ACTH, cortisol,
CRH, epinephrine, and norepinephrine), immune cell chemical messengers
called
cytokines (interleukins),
additional hormones (androgens, estrogens, progesterone, and growth hormone),
and neuropeptides.
Neuropeptides are chains of amino acids, like
beta-endorphins, that neurons use for communication.
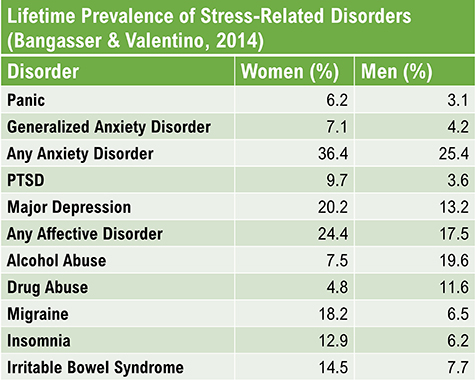
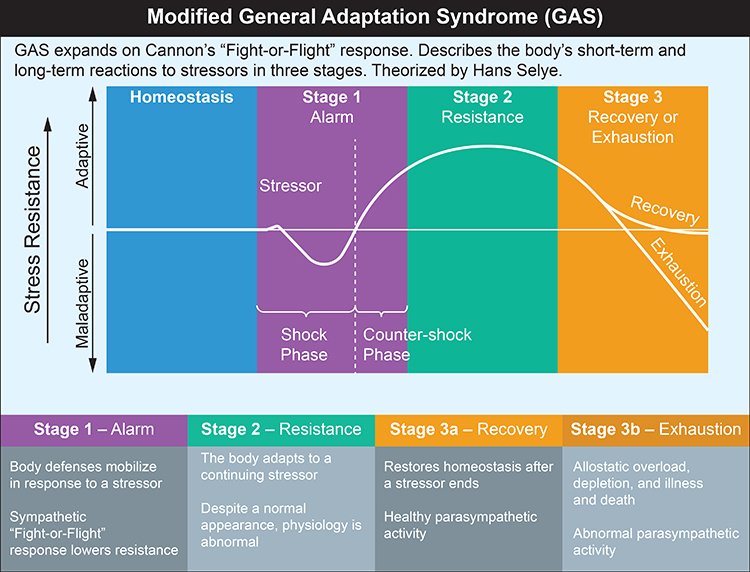
Stress and Immunity
There is persuasive evidence that stressful life events can reduce
immunity and that behavioral interventions can enhance or maintain it.
Bereavement can reduce lymphocyte (lymphatic white blood cell)
proliferation (Schleifer et al., 1983). Academic exams, marital
conflict, negative affect associated with stress, clinical and
subclinical depression, and negative daily mood can suppress immunity
(Herbert & Cohen, 1993; Kiecolt-Glaser et al., 2002; Stone et al.,
1994).
The stress of living near the Three Mile Island nuclear plant when it
experienced a significant accident reduced residents' B cell, T cell, and
natural killer cell counts compared with control subjects (McKinnon
et al., 1989).
A study of Alzheimer's caregivers showed lowered immunity and longer
wound healing times, and worse psychological and physical health than
controls who were not caregivers (Kiecolt-Glaser, 1999). The
Alzheimer's patients' deaths did not improve caregiver immunity or
psychological functioning (Robinson-Whelen et al., 2001).
Finally, laboratory stressors produced more significant discomfort and
immunosuppression in chronically-stressed young males than in those not chronically stressed (Pike et al., 1994). Exposure to chronic
stress may have intensified their subjects' response to acute laboratory
stressors.
Behavioral Interventions Can Strengthen Immunity
Behavioral interventions can increase immunocompetence. Miller and Cohen's (2001)
meta-analytical study of behavioral interventions showed modest
increases in immunity. Hypnosis increased immune function more than
relaxation and stress management.
A stress management program incorporating relaxation training
reduced symptoms and increased salivary antibodies and psychological
functioning in children diagnosed with frequent upper respiratory
infections (Hewson-Bower & Drummond, 2001).
College students who wrote journal entries about highly stressful
experiences increased lymphocyte proliferation and made fewer health
center visits (Pennebaker et al., 1988). Smyth et al.
(1999) asked asthma and
rheumatoid arthritis patients to write journal entries about highly
stressful experiences or planned daily activities. At a 4-month
follow-up, 50% of the Pennebaker journal group who wrote about stressful
experiences and 25% of the control group achieved clinically significant
improvement in their immune-related disorders (Crider, 2004).
Dental and medical students who received hypnosis training maintained
immune function, while a control group showed declines in immunity (Kiecolt-Glaser
et al., 2001). This finding suggests that behavioral interventions may be more
effective in maintaining normal immunity than boosting immunity (Brannon et al., 2022).