Today, I am going to introduce you to a method that will help you control your symptoms. We will be using a number of measuring devices, and wearing them may feel a little strange in the beginning. This introduction will allow you to become familiar with what it feels like to wear the sensors, and to watch the body signals they are measuring on the screen, before we start your biofeedback training. I will attach all of the sensors to your body and then you will see what they are measuring on your monitor. These sensors will simply be measuring your physiological activity and will not cause any harm to you. I will briefly explain what each measurement is (p. 98). Attach and test each sensor, start displaying physiological activity, and explain the meaning of the graphs and numerical values. For example: In this top graph, the red line is your heart rate in terms of beats per minute, and the blue line shows your breathing. You’ll notice that the blue line moves up as you breathe in and down as you breathe out (p. 99).
Resonance Frequency Assessment
The resonance frequency is a fixed characteristic of an adult's cardiovascular system that reflects the blood volume in the vascular tree (Vaschillo et al., 2002, 2006).
Graphic © Design_Cells/Shutterstock.com.
Practitioners use resonance frequency (RF) and slow-paced breathing protocols to teach clients to increase heart rate variability (HRV). Both strategies increase respiratory sinus arrhythmia (RSA), which stimulates the baroreceptor reflex and vascular tone rhythm to increase HRV. Graphic © BioSource Software LLC.
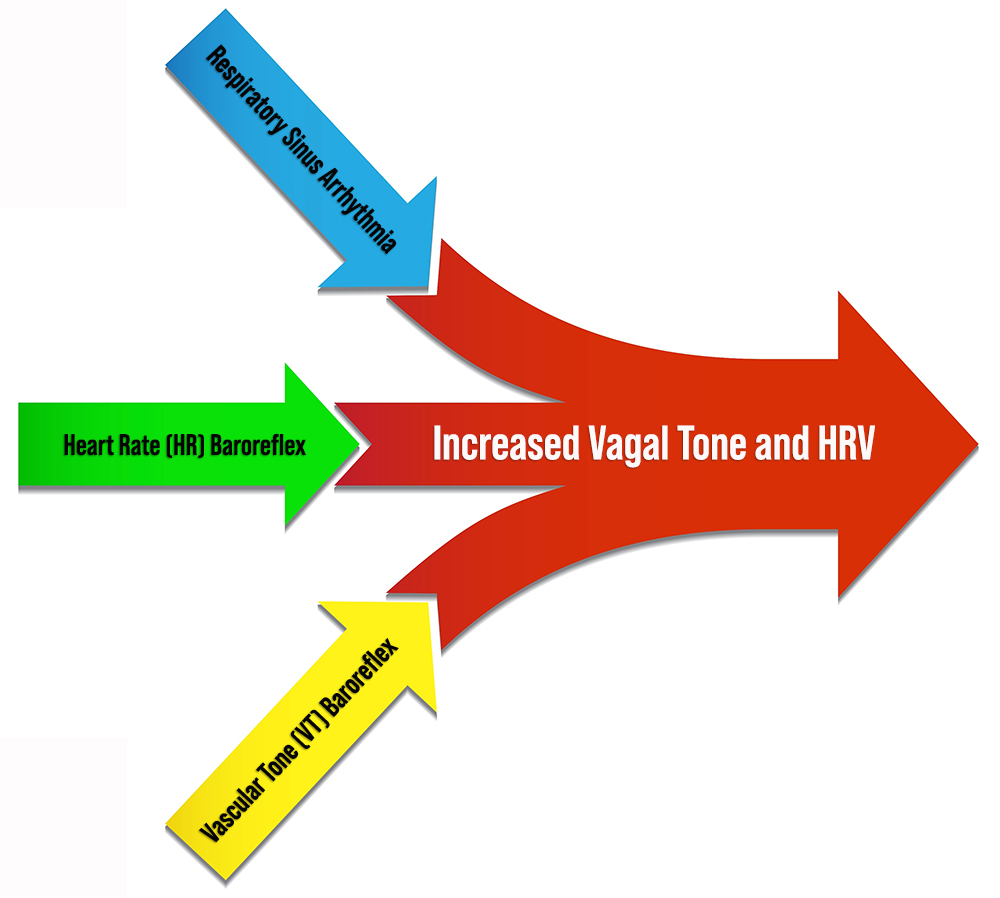
For the cardiovascular system, the resonance frequency (RF) is the rate at which it can be stimulated to produce the greatest RSA amplitudes, HRV, and baroreflex gain (Lehrer, Vaschillo, & Vaschillo, 2000). Baroreflex gain is heart rate (HR) change per 1 mmHg change in blood pressure (BP; Lehrer & Gevirtz, 2014).
The mechanisms underlying this amplification process are complex:
The mechanism for this effect lies in a confluence of processes: (1) phase relationships between heart rate oscillations and breathing at specific frequencies, (2) phase relationships between heart rate oscillations and breathing at specific frequencies, (3) activity of the baroreflex, and (4) resonance characteristics of the cardiovascular system (Lehrer & Gevirtz, 2014, p. 1).The graphic below, adapted from Gevirtz et al. (2016), illustrates a 4- to 10-fold RSA increase from breathing at typical rates to RF breathing (Vaschillo et al., 2002; Lehrer et al., 2020b).
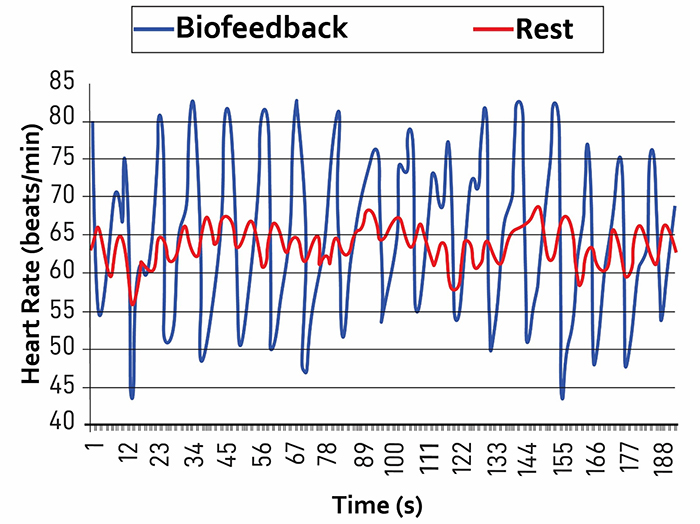
Note: The red waveform shows HR oscillations while resting without breathing instructions or feedback. The blue waveform shows HR oscillations with HRV biofeedback and breathing from 4.5-6.5 bpm.
RF assessment aims to identify the approximate stimulation rate that produces the strongest resonance effects (RSA).
The RF model assumes that the RF ranges between 4.5 and 6.5 times/minute for adults and 6.5-9.5 times/minute for children and that training near the RF will produce the greatest RSA and HRV (Lehrer et al., 2013; Lehrer & Gevirtz, 2014).Appreciation
Lehrer et al. (2013) developed the original RF measurement protocol. We recommend their excellent article on HRV biofeedback training in Biofeedback.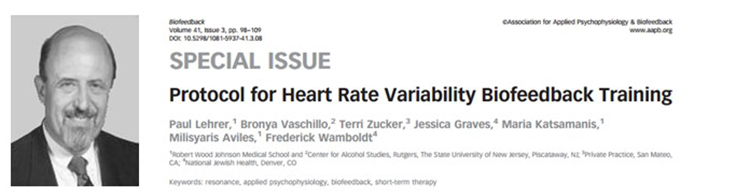
We also enthusiastically recommend Lehrer and Gevirtz's Frontiers HRV biofeedback overview.

Didier Combatalade, Director of Clinical Interface at Thought Technology Ltd., provided invaluable technical support in measuring the phase relationship between respirometer and heart rate signals using BioGraph Infiniti software.

Christopher Zerr, Washington University Cognitive Neuroscience postdoctoral fellow, provided technical support and supervised data collection to illustrate this protocol.
BCIA Blueprint Coverage
This unit addresses V. HRV Biofeedback Strategies: C. How to measure the resonance frequency.
Professionals completing this unit will be able to discuss:
A. The meaning of resonance frequency
B. Resonance frequency assessment

This unit covers the Resonance Frequency Measurement Protocols, Fine-Tuning the Resonance Frequency, An Alternative Method to Find the Resonance Frequency, and Unanswered Questions.
Please click on the podcast icon below to hear a full-length lecture.

Resonance Frequency Measurement Protocols
Start with Breathing Assessment
RF measurement protocols require that clients breathe continuously and smoothly at slower-than-typical rates. Breathing assessment can identify rapid breathing and dysfunctional behaviors that could interfere with RF determination. Asthma, Generalized Anxiety Disorder, low back pain, and dysfunctional breathing behaviors like overbreathing may be associated with rapid breathing. Postpone RF assessment for adults until you successfully train them to breathe effortlessly (Peper et al., 2008) between 4.5 and 6.5 bpm.Resonance Frequency Assessment Concerns and Contraindications
Some clients may find slow-paced breathing difficult. They may overbreathe and expel excessive CO2. If they report symptoms of feeling faint or rapid heartbeats, encourage them to take shallower and smoother breaths (Lehrer et al., 2013).Resonance frequency assessment is contraindicated for clients whose sinus rhythm is driven by a pacemaker because this device externally regulates HRV. Do not assess clients whose overbreathing compensates for increased acidity in the blood due to conditions like kidney disease. Slow-paced breathing would increase CO2 levels in the blood and dangerously increase acidosis (Khazan, 2013).
Sensor Channels and Parameters Monitored
Resonance frequency measurement requires the display of instantaneous HR and respiration in real-time.ECG or PPG Methods
A clinician monitors HR using an electrocardiograph (ECG) or a photoplethysmograph (PPG). ECG and PPG sensors obtain similar interbeat interval (IBI) values under resting conditions with healthy blood flow (Giardino et al., 2002; Schafer & Vagedes, 2013). However, PPG monitoring from the toes, thumb, and earlobes increasingly lags behind the ECG during slow-paced breathing. Phase delay is symmetrical between corresponding recording sites (e.g., left and right index fingers; Allen, 2019).During resting conditions after 1 minute of deep breathing, PPG recordings from the earlobe agree with ECG measurements (Weinschenk et al., 2016). However, the PPG method may be less accurate during slow-paced breathing (Jan et al., 2019) and marked sympathetic activation. Disorders such as anxiety are associated with peripheral vasoconstriction that interferes with detecting the pulse from the digits. In contrast, vasoconstriction does not affect ECG detection of R-spikes from the chest, torso, or wrists (Giardino et al., 2002; Schafer & Vagedes, 2013; Shaffer & Combatalade, 2013).
To determine which method is more appropriate, a clinician should evaluate whether the raw PPG waveform is flat or low-amplitude (Shaffer & Combatalade, 2013).
Respirometer
Respiratory feedback serves multiple functions during RF assessment as adults breathe from 6.5 to 4.5 bpm in 0.5-bpm steps: pacing, respiration rate (RR) confirmation, and identification of dysfunctional breathing.A respiration display guides clients to breathe at prescribed rates and confirms their success. Both actions are critical because we cannot evaluate the effects of breathing at 5.5 bpm if a client actually breathed at 6 bpm. Respiratory monitoring is also essential to identify dysfunctional breathing behaviors like apnea (breath-holding) and overbreathing (excessive exhaling of CO2), which can interfere with HRV biofeedback.
Clinicians use a respirometer, a flexible sensor band that measures abdominal or thoracic movement to detect the respiratory waveform (Shaffer & Moss, 2019). Graphic © BioSource Software LLC.

A clinician should continuously monitor all raw waveforms (ECG or PPG and respirometer) for artifacts (false values) during each slow-paced breathing trial so that they can immediately repeat failed trials.
Orientation for RF Assessment
The resonance frequency assessment protocol (Lehrer et al., 2013) described in this article provides intuitive directions.
A clinician invites questions and provides a brief overview of the RF assessment procedure before starting practice trials. They adjust the explanation to match a client's understanding (Lehrer et al., 2013).

Today we are going to find out the speed of breathing that should best help you to cope with your symptoms. This breathing frequency is different for each person. When you breathe at this rate, your breathing will produce strong effects on your nervous and cardiovascular systems that should be very good for you and should help you to control your symptoms (p. 99). Your heart rate varies with each breath, and with various other processes in your body, including the baroreflex. This variability is good and is a sign of health. We will now find your “resonance frequency” – the speed of breathing at which your HRV is the highest. In this task, we will ask you to breathe at five rates for periods of about 2 min each. You should not find this task difficult. However, if you feel uncomfortable at any time, you can simply stop the task and tell us. When we begin, we will ask you to breathe in and out at a 10-s breathing rate. Then we will ask you to breathe at various other rates, so we can find the exact frequency at which your cardiovascular system resonates. This will be your own resonance breathing frequency. You will be able to use this breathing rate to best help your symptoms. Breathe easily and comfortably, but not too deeply. Do not try too hard. Do you have any questions? (p. 99).
Practice Breathing Trials
Before starting RF trials, clinicians should provide their clients with breathing practice because the protocol requires slower-than-normal breathing rates. This precaution is crucial for clinical populations such as clients diagnosed with chronic pain. Although a healthy resting adult breathes from 12 to 20 bpm (Khazan, 2019a), a RF assessment protocol instructs adults to breathe at less than half that rate.Allow clients to practice healthy breathing from 5.5 to 6 bpm before starting RF trials. When a RR is difficult, instruct them to increase or decrease it by 1/2 bpm. For example, if a client typically breathes at 18 bpm, instruct them to decrease their breathing rate every few seconds from 18 bpm to 17.5 bpm to 17 bpm, and so forth.
Standardize the inhalation-to-exhalation ratio across breathing trials. Longer exhalation than inhalation is recommended in RF assessment (Lehrer et al., 2013) and may increase RSA from baseline values due to a greater increase in cardiac vagal tone (Strauss-Blasche et al., 2000; Van Diest et al., 2014). However, several studies (Zerr et al., 2015; Meehan et al., 2017) found no difference between resting HRV metrics (e.g., HR Max-HR Min, pNN50, RMSSD, SDNN, and LF power) when participants breathed at 1:1 and 1:2 inhalation-to-exhalation ratios.
Stepped Protocol
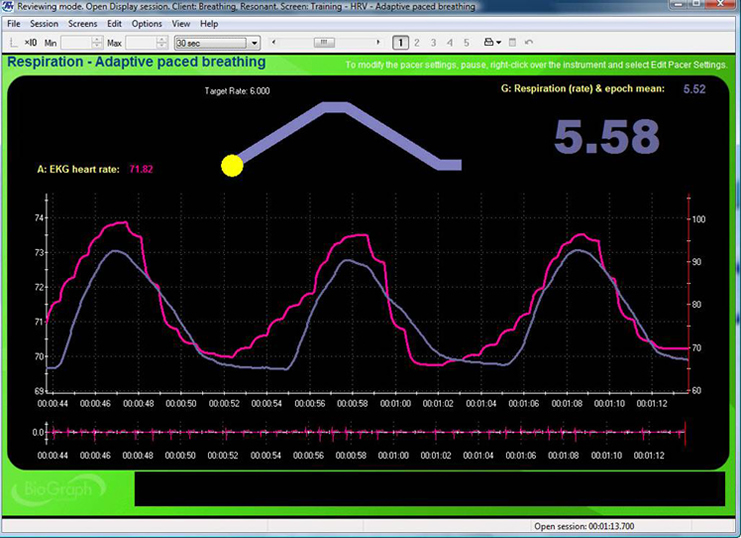
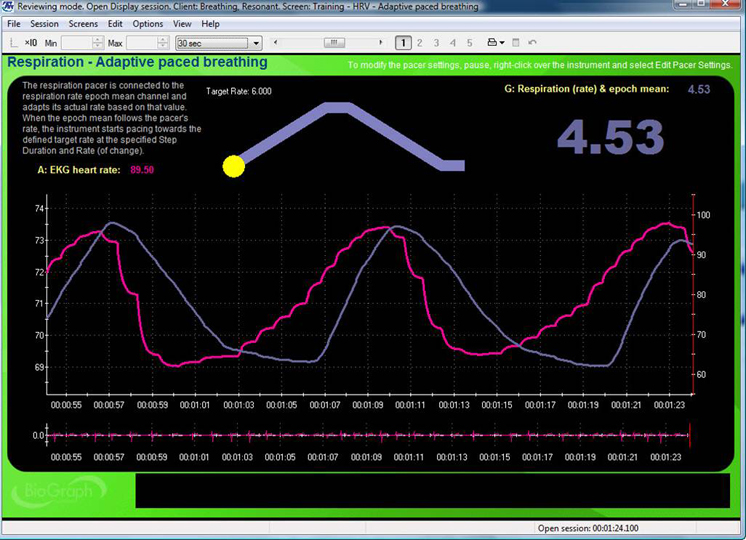
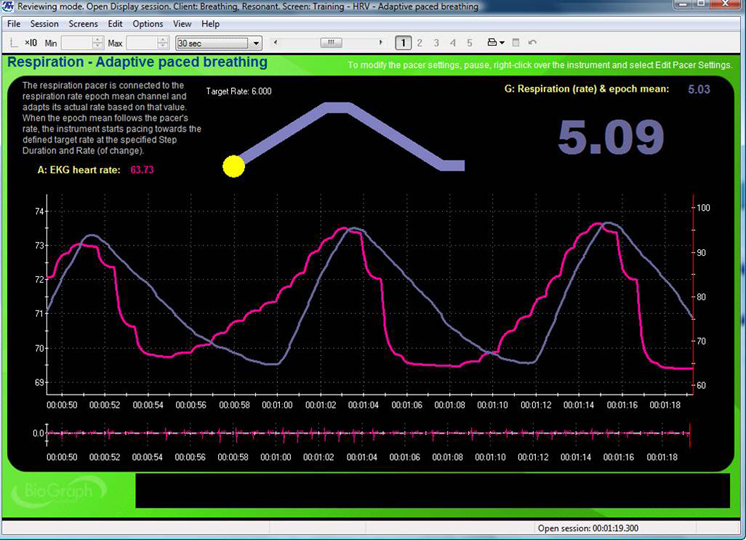
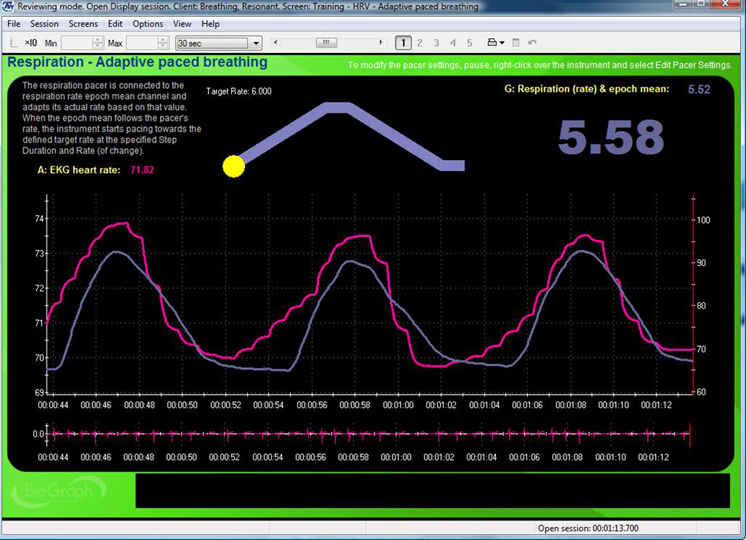
Instruct your client to breathe for 2-minute intervals from 6.5 to 4.5 bpm, decreasing in 0.5 bpm steps with 2-minute rest periods. Record physiological activity during slow-paced breathing as separate 2-min epochs. Create a separate display for each RF trial and capture 2 minutes of raw breathing and HR waveforms on the same graph for each RR.The top display with the moving yellow ball is designed to help clients breathe at 6 bpm. A post-expiratory pause follows the exhalation. The current respiration rate (5.58 bpm) appears on the right. The graph immediately below shows instantaneous heart rate (pink) and respiration (purple). Note the degree to which the waveform peaks and troughs coincide since this graphically represents phase synchrony. A raw ECG waveform is displayed toward the bottom of the screen. Graphic © BioSource Software LLC.
Consider the following directions when introducing each RR: “Now try breathing at this frequency (following the pacer)” (Lehrer et al., 2013, p. 101).
After your client completes 2 minutes of paced breathing, check on their comfort and verify that they followed the pacer by confirming the average RR for that trial. Repeat trials if the clients were 0.25 bpm too fast or slow. Assessment without a respirometer lacks this quality control. We cannot verify that clients have breathed at the target rates in these cases. Check for artifactual IBIs and repeat invalid epochs after the client has rested for 2 minutes. Examine the segment spectral display for the location of LF peaks. When a peak occurs at 4.5 or 6.5 bpm, extend assessment with trials 0.5 bpm above and below this inflection point until LF amplitude decreases.
Resonance Frequency Selection
Dr. Lehrer explains how to determine the resonance frequency © Association for Applied Psychophysiology and Biofeedback. You can enlarge the video by clicking on the bracket icon at the bottom right of the screen. When finished, click on the ESC key.RF selection aims to identify the frequency that best stimulates the baroreflex system, increasing RSA and HRV. The Lehrer and colleagues (2013) protocol estimates a client's approximate RF because its resolution is limited to 0.5-bpm steps. When a client's actual RF is 5.75 bpm, both 5.5 and 6.0 bpm could maximize different RF selection criteria.
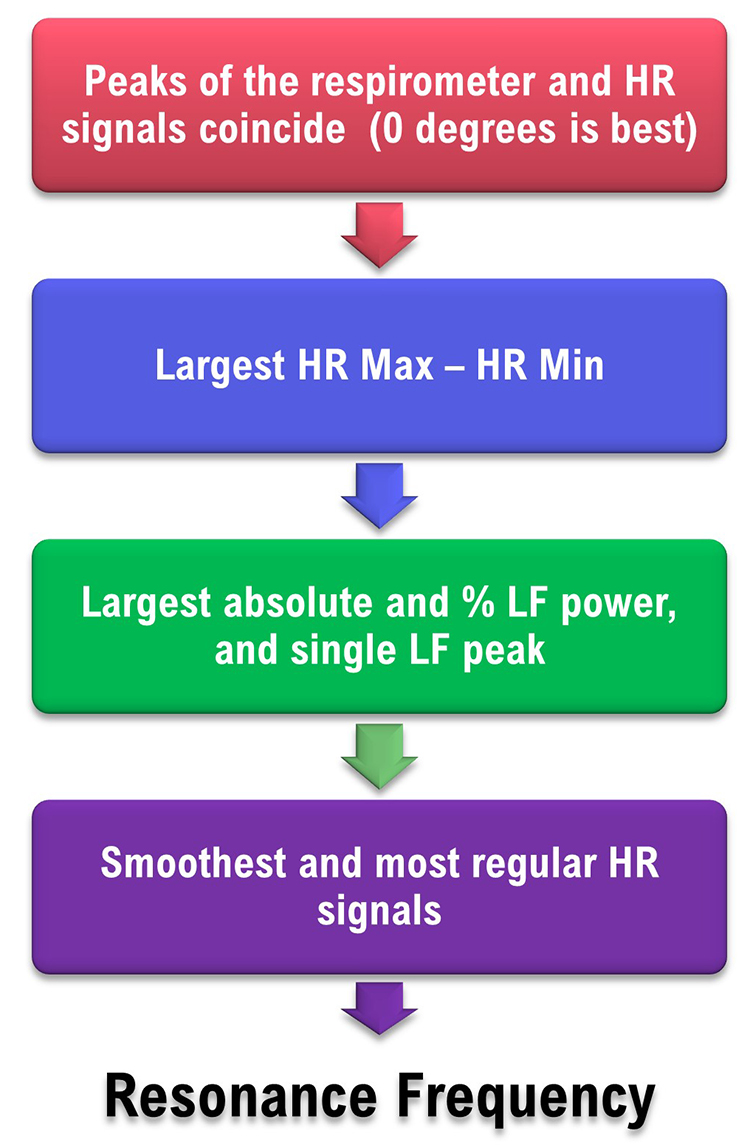
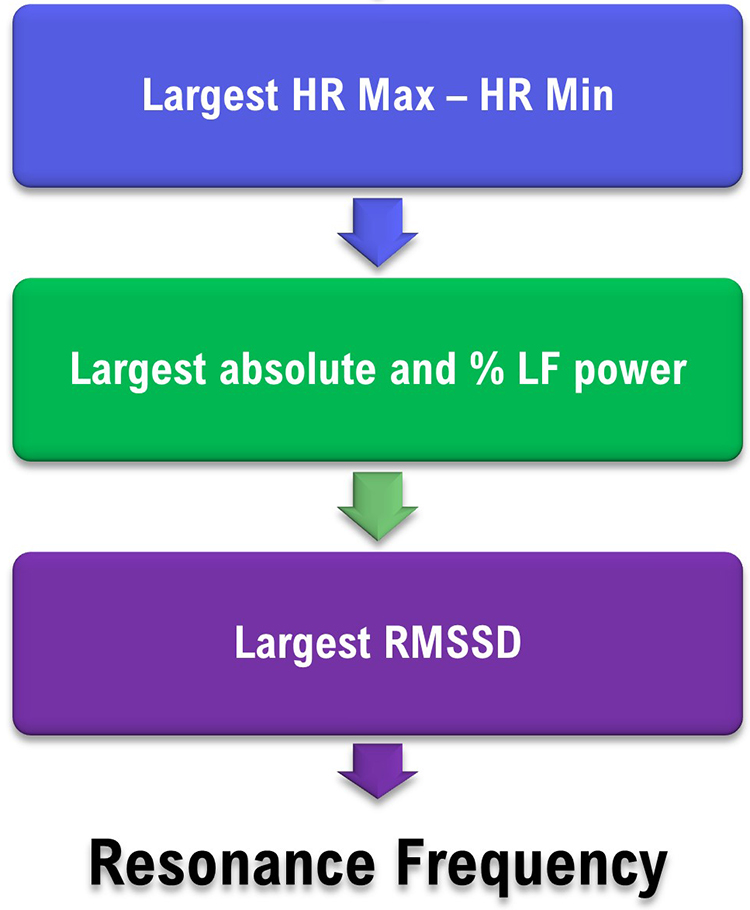
The Lehrer and colleagues strategy incorporates six criteria which are prioritized by their association with resonance effects. Since a single breathing rate may not maximize all six criteria, clinicians select the estimate representing the “best convergence” of the selection criteria (Lehrer et al., 2013, p. 102). These criteria and their weights require experimental confirmation (Shaffer & Meehan, 2020).

(1) Phase Synchrony
In adults, when respiration and HR signals rise and fall simultaneously (0°), this maximally stimulates the baroreflex and increases RSA (Vaschillo et al., 2004; Lehrer & Gevirtz, 2014; Lehrer et al., 2020a). Whether RSA optimizes pulmonary gas exchange efficiency is currently unclear (Buchheit, 2010). The software measures the phase synchrony between the respirometer and HR waveforms: 0° means that HR begins to rise at the start of an inhalation; 90° means that HR begins to increase during the middle of an inhalation and to decrease during the middle of an exhalation; 180° means that HR decreases during inhalation and increases during exhalation.Phase synchrony (~0°) carries the greatest weight because it enables clients to achieve the greatest resonance effects. Strong resonance effects, in turn, increase RSA and many HRV metrics and allow HRV biofeedback training to more effectively stimulate and strengthen the baroreflex (Lehrer et al., 2003, 2013; Shaffer & Meehan, 2020).
(2) HR Peak-Trough Amplitude
Higher HR peak-trough amplitudes are better because greater RSA can increase baroreflex sensitivity over weeks of HRV RF training (Lehrer et al., 2003; Lehrer & Gevirtz, 2014). HR Max – HR Min is one way to quantify peak-trough amplitude (Cipresso et al., 2019). Clinicians measure HR Max – HR Min using a respirometer to determine when each breathing cycle starts and ends. Peak-trough amplitude is second because larger peak-trough differences signal greater resonance effects and contribute to more effective baroreflex activation (Vaschillo et al., 2002; Shaffer & Meehan, 2020).(3) Low-Frequency Power
The baroreflex system exhibits resonance because it is a feedback system with a constant delay (Lehrer, 2013). Its RF lies within the LF range. Higher absolute and percent total LF power are desirable because they increase as the RR approaches the RF and more effectively stimulates the baroreflex (Vaschillo et al., 2002). Further, cardiac vagal activity increases when individuals engage in slow-paced breathing within the LF range (Kromenacker et al., 2018). Clinicians measure absolute LF power of the 0.04–0.15 Hz range in ms2/Hz. They calculate the percent total LF power as LF/(LF + HF) or LF/(VLF + LF + HF; Lehrer et al., 2013). LF power is third because it confirms that clients are breathing at rates between 4.5 and 6.5 bpm, which are necessary to produce the greatest resonance effects and possibly RSA (Shaffer & Meehan, 2020).(4) Maximum LF Amplitude Peak
Larger LF peaks reflect stronger resonance effects due to greater synchrony between breathing and HR. Clinicians use spectral analysis to identify the LF peak with the largest absolute power. The maximum LF amplitude peak is fourth because the LF spectral peak is higher at the RF than at any other respiratory frequency (Lehrer et al., 2013). When clients breathe consistently within the LF range, this increases resonance effects and RSA (Shaffer & Meehan, 2020).(5) Smoothness of the HR Curve Envelope
Smooth heart rate waveforms are best because they permit closer phase synchrony with respiration waveforms and allow clients to achieve the greatest resonance effects and RSA (Lehrer and Gevirtz, 2014). Clinicians visually inspect HR curve envelope for their smoothness. Sinusoidal signals are smooth, whereas jagged waveforms are irregular (Lehrer et al., 2013). The smoothness of the HR curve envelope is fifth because it reflects the breathing mechanics required to achieve the greatest resonance effects and RSA (Shaffer & Meehan, 2020).(6) Fewest LF Peaks
Fewer peaks are better than more peaks because they are generated by breathing within a narrower frequency band about the RF within the LF range. Clients can generate multiple peaks when they breathe slightly faster or slower than their RF. This can result in a peak at the respiratory rate and another at the baroreflex frequency. In contrast to breathing at various frequencies in the LF range, breathing at a single frequency better enables phase synchrony between breathing and HR, stimulates the baroreflex, and increases RSA (Vaschillo et al., 2002). Clinicians can count the number of LF peaks by visually inspecting a spectral display of the LF range. The fewest LF peaks is sixth because this demonstrates that the client is consistently breathing within a narrow band within the LF range, which increases resonance effects and RSA (Shaffer & Meehan, 2020).The table below is adapted from Lehrer and colleagues' (2013) RF assessment protocol.
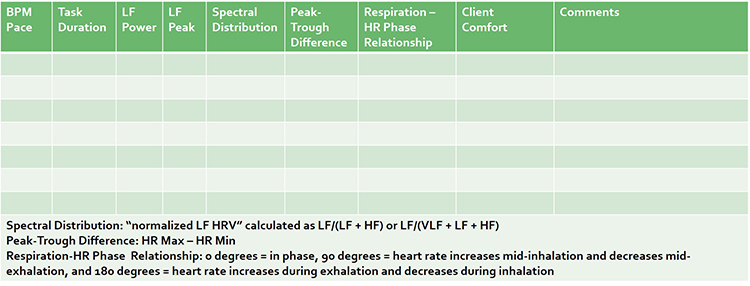
Resonance Frequency Selection Criteria
The RF is the breathing rate that represents the “best convergence” of these criteria (Lehrer et al., 2013, p. 102):1. synchrony of the respirometer and HR signals
2. largest peak-to-trough HR amplitude
3. largest absolute and percentage LF power, and highest amplitude LF peak frequency near 0.1 Hz
4. smoothest and most regular HR waveforms
Selecting the RF Using Actual Data
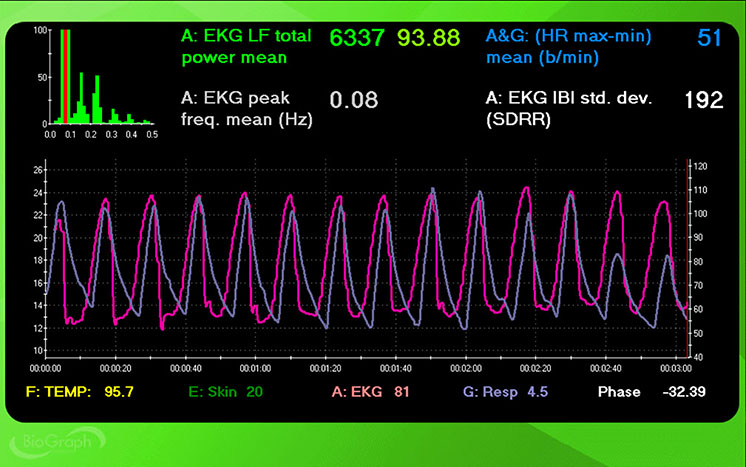
Using the Lehrer et al. (2013) criteria, we might choose a respiration rate of 5.5 bpm due to its synchrony (7o), peak-to-trough difference (49 bpm), HR curve envelope smoothness (+), and the number of LF peaks (+).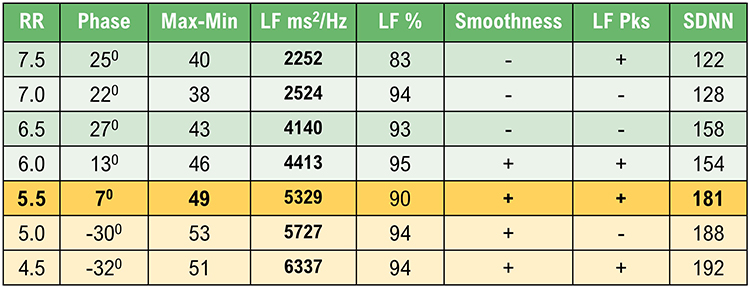
However, a clinician could also make a case for 5.0 and 4.5 bpm. Despite dramatically worse phase, 5.0 and 4.5 bpm achieved higher peak-to-trough differences (53 and 51 bpm), LF power (5727 and 6337 ms2/Hz), LF % (both 94), and SDNN (188 and 192 ms) than 5.5 bpm.
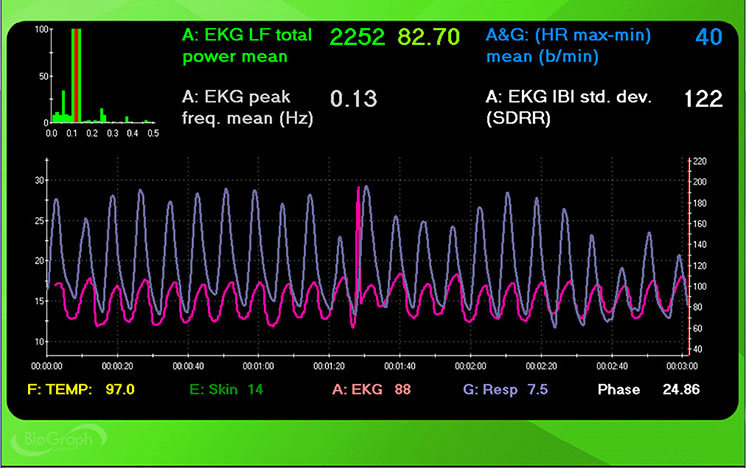
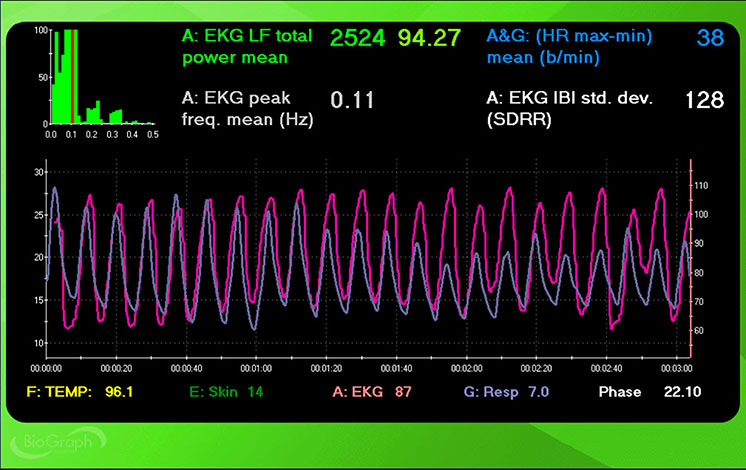
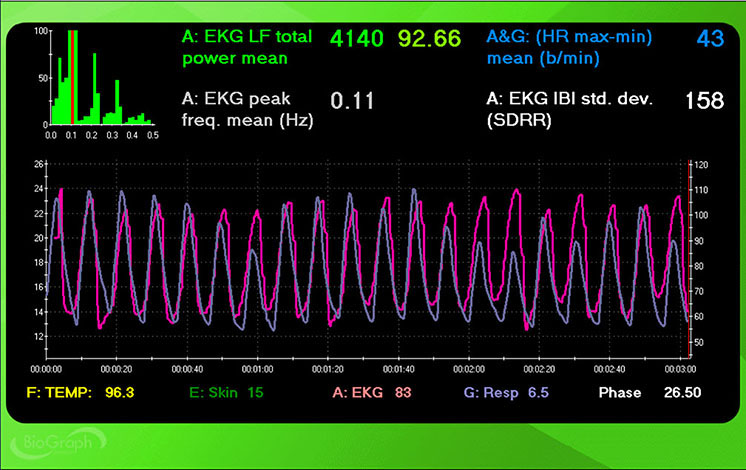
Screenshots for each breathing trial (7.5 to 4.5 bpm) display HR and respiration waveforms. The pink tracing shows instantaneous HR, and the violet tracing shows respirometer expansion and contraction.

7.5 bpm
7.0 bpm
6.5 bpm
6.0 bpm
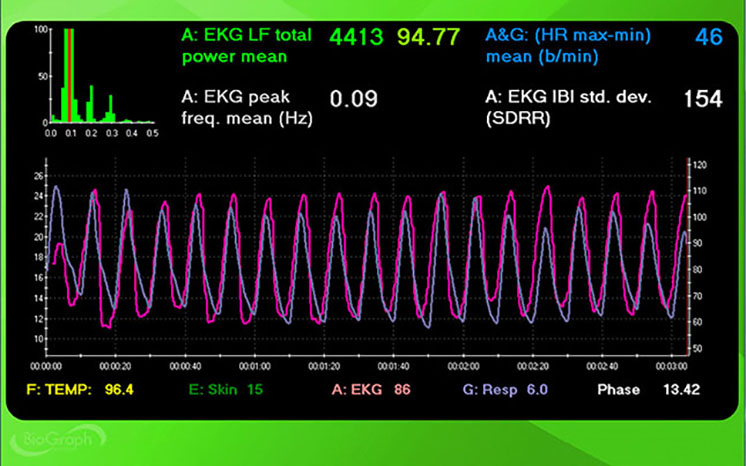
5.5 bpm
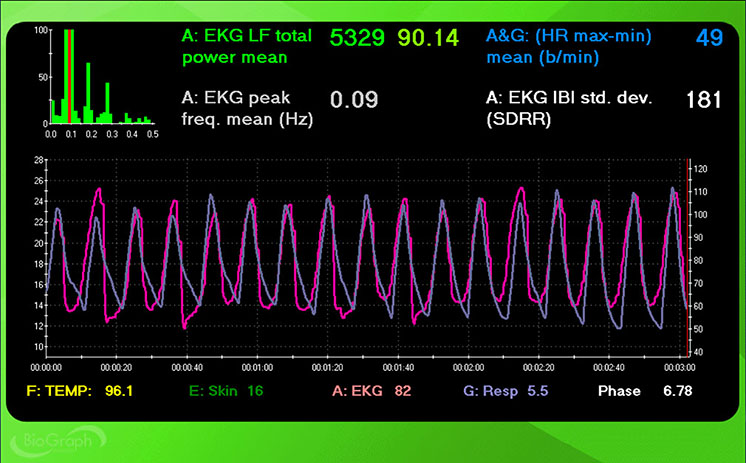
5.0 bpm
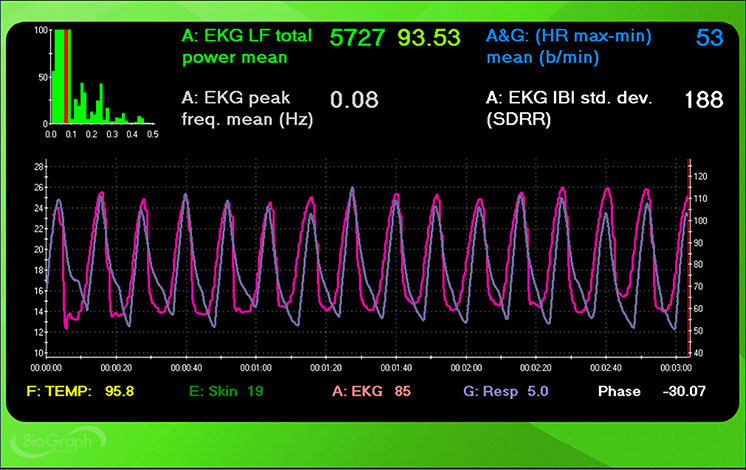
4.5 bpm
How to Break Ties
Although slow-paced breathing at 5.5, 5.0, and 4.5 should increase RSA and HRV, selecting the rate your client finds most comfortable and rewarding is critical. A client-friendly rate will increase your client's likelihood of practicing RF breathing. For example, if your client struggles with breathing at 4.5 bpm, this pace may result in overbreathing and vagal withdrawal, discomfort, and reduced engagement (Porges, 1995; Thayer et al., 2012).Also, consider which rate brings your clients closest to their training goal? If your clients entered training to reduce BP, consider the frequency that produces the lowest readings.
How to Fine-Tune the RF

Following a resting baseline at the start of the first training session, clinicians should monitor 3–5 min of breathing at the RF while watching for signs of overbreathing like faintness and tingling of the extremities (Lehrer et al., 2013). If such symptoms are present, clinicians should encourage shallower breathing to reduce the CO2 loss responsible for them.
Next, they should ask clients to breathe at 1/2-bpm faster and slower rates for 3–5 min each. This step allows clients to compare their subjective comfort one more time during each breathing rate. Finally, after artifacting, clinicians should evaluate the three trials – RF, RF + 1/2-bpm, and RF - 1/2-bpm – using the previous RF criteria.
Stepped Protocol Difficulties
Slow-paced breathing can be challenging for clients who breathe at average or higher-than-typical rates. In addition to slowing their RR, the RF protocol may ask them to lengthen their exhalation. Although clients may breathe at the target rate on average during RF trials, they may not consistently follow the pacing display.Variability around each target RR could compromise most of the selection criteria. Specifically, these fluctuations could reduce phase synchrony, lower the maximum LF peak, decrease the smoothness of the HR curve envelope, and increase the number of LF peaks. These criteria appear to measure slow-paced breathing proficiency rather than baroreflex frequency.

Perhaps the largest peak-trough amplitude and LF power (absolute and percentage) should be the primary RF criteria since they are less affected by breathing proficiency. Also, since RMSSD is a robust short-term HRV index, it should be evaluated as the third criterion. We present a simplified decision flowchart to stimulate conversation and research.
Sliding Protocol
Fisher and Lehrer (2022) described a 15-min automated sliding protocol in which participants breathed between 4.25 and 6.5 bpm, with a constant 67.04-ms rate of change. Since peak-trough amplitude proportionally increases as clients approach the RF, the sliding protocol measures this metric at 78 frequencies. In contrast to the subjectively weighted multiple criteria of the stepped approach, the sliding protocol identifies the frequency with the largest peak-trough amplitude.The mean absolute difference in RF between the two methods was 0.22 ± 0.169 bpm. The authors raise the issue of whether this slight difference between RF estimates is too small to affect physiological or psychological outcomes.
Alternative Methods to Find the RF Using emWave Pro Plus ®
Clinicians can use this method for distance HRV biofeedback training. A limitation is that the absence of a respirometer prevents confirmation that a client breathed at the required rates. This modified protocol uses an integrated or external breathing pacer.

You will need to visually confirm client success in following a pacer utilizing a webcam by counting breaths over each 2-minute period. We will describe an approach using the emWave Pro Plus ®.
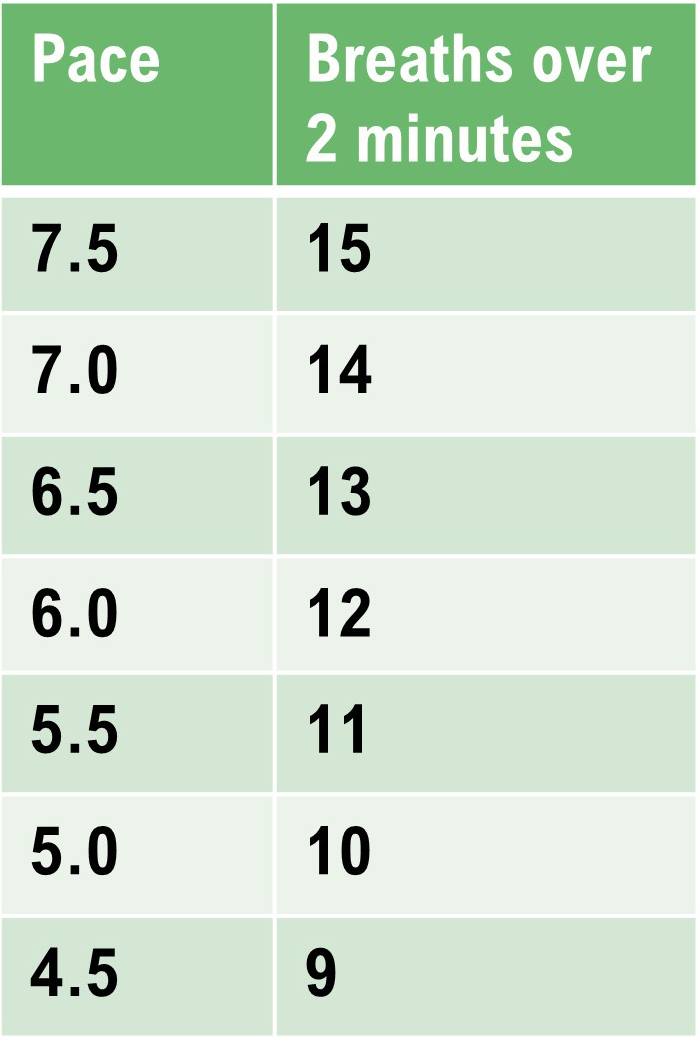
Method 1: emWave Pro Plus ® with a separate smartphone pacer
Perform a series of 2-minute Assessments using the emWave Pro Plus® and a separate breathing pacer while the client sits upright. Adults will breathe from 7.5 to 4.5 bpm in descending 0.5 bpm steps. Use 9.5 to 6.5 bpm for children. After each 2-minute trial, inquire about hyperventilation symptoms like feeling lightheaded, dizzy, or having a pounding heart. Set the emWave Pro Plus Assessment for 2 minutes.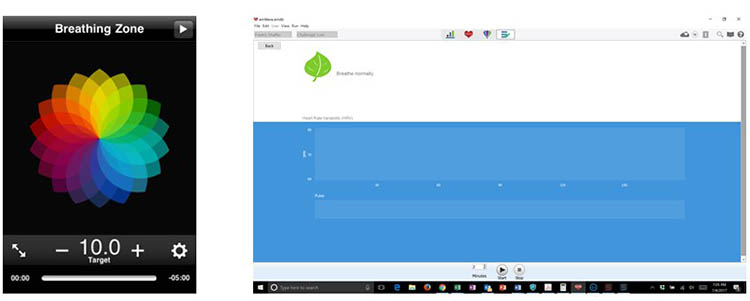
After completing the 2-minute Assessments, visually inspect the data points to ensure that emWave Pro Plus has deleted all false beats (shown by a circled red x). Below, there are two false beats near the top of the tachogram, around 14 seconds and 53 seconds. Use Edit to delete any overlooked false beats.

After you complete artifacting, run a separate report for each trial. Then, compare the HR tachograms and summary statistics. Compare the HR tachograms and HRV measurements for each breathing trial on separate PowerPoint slides or a Word document.
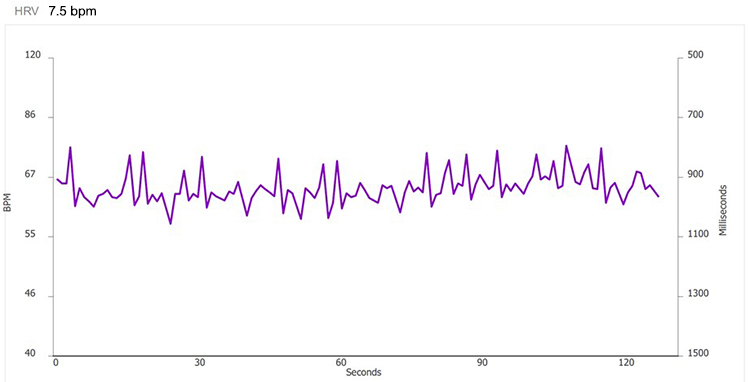
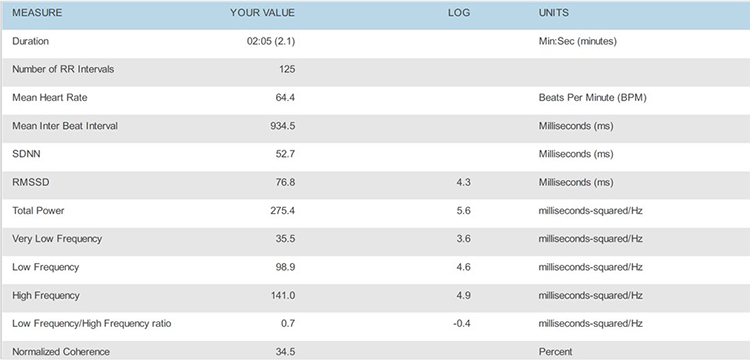
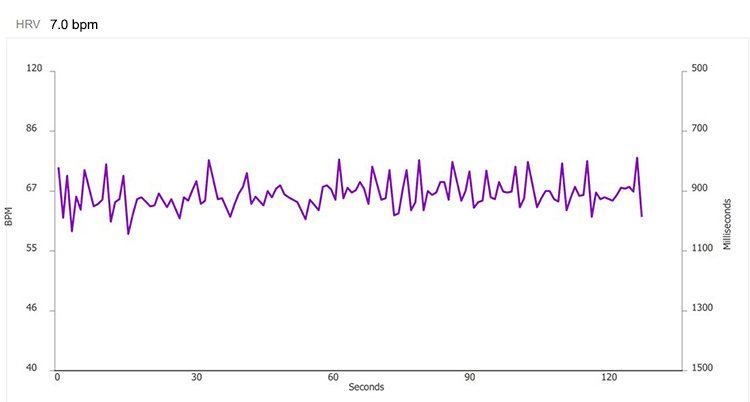
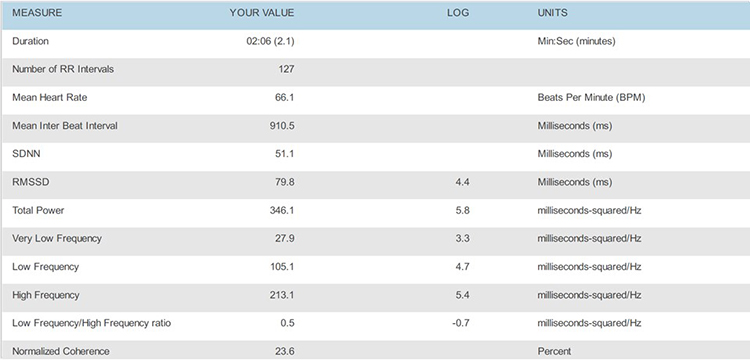
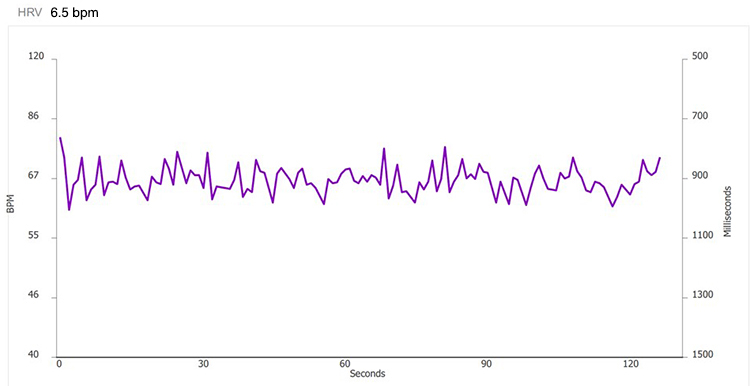
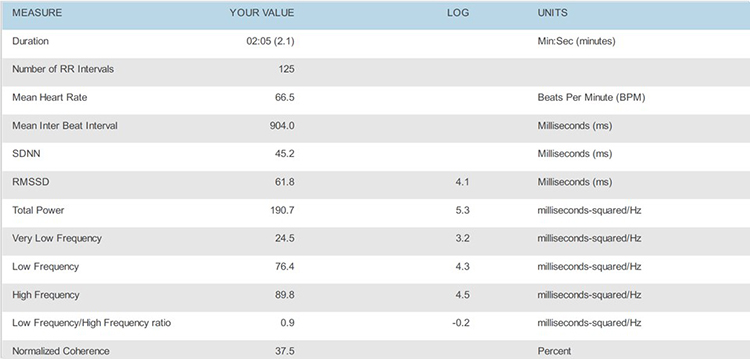
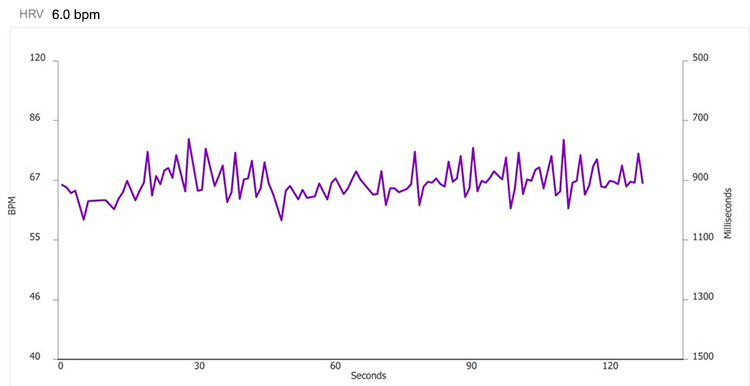
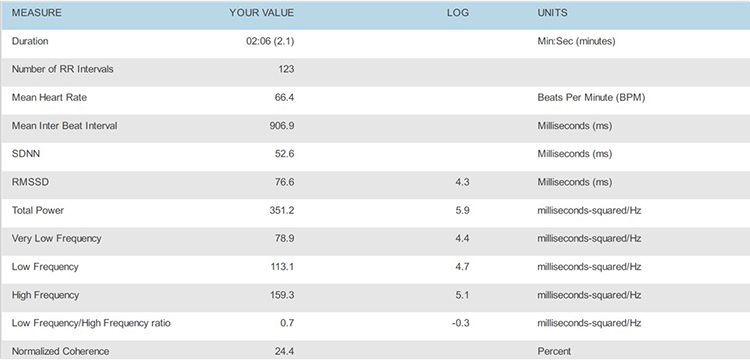
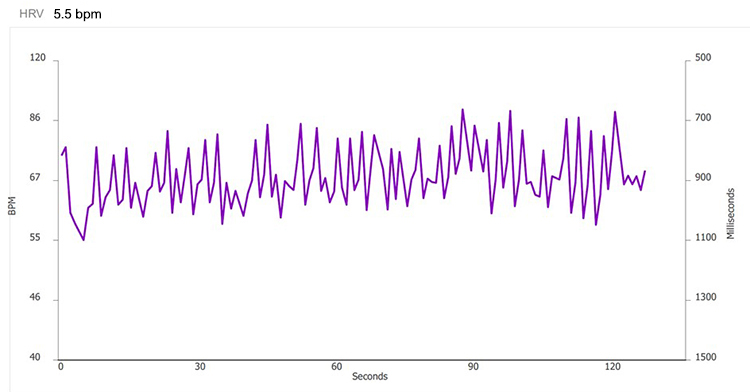
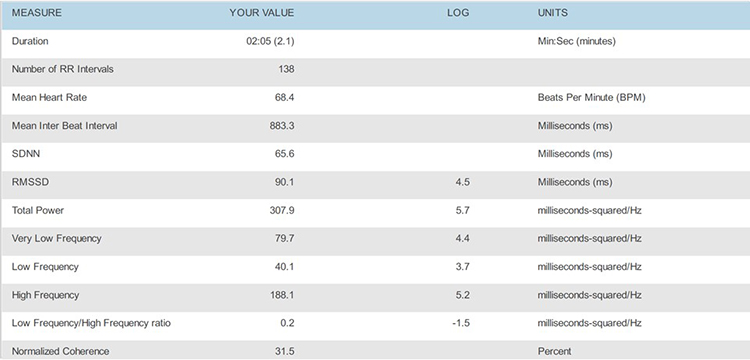
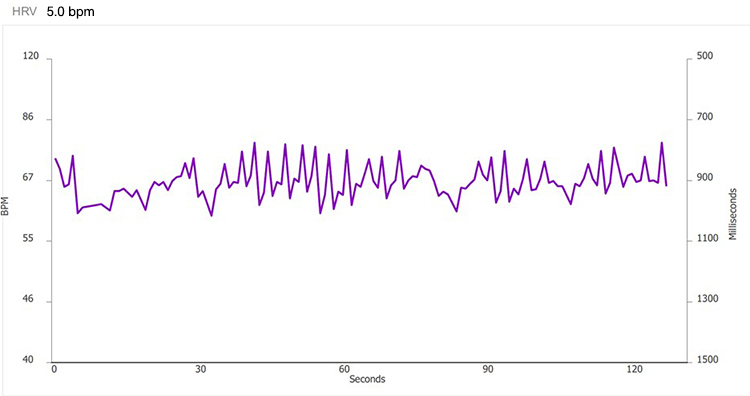
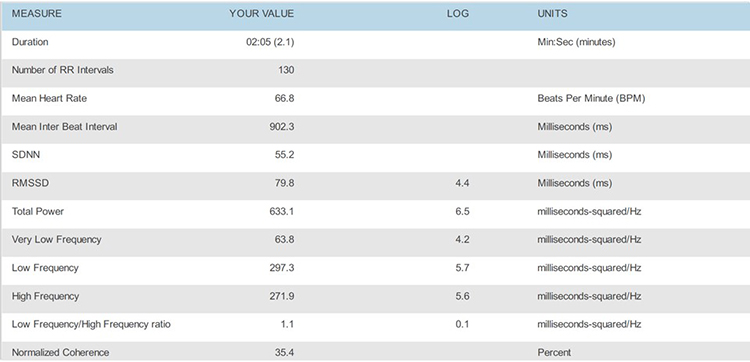
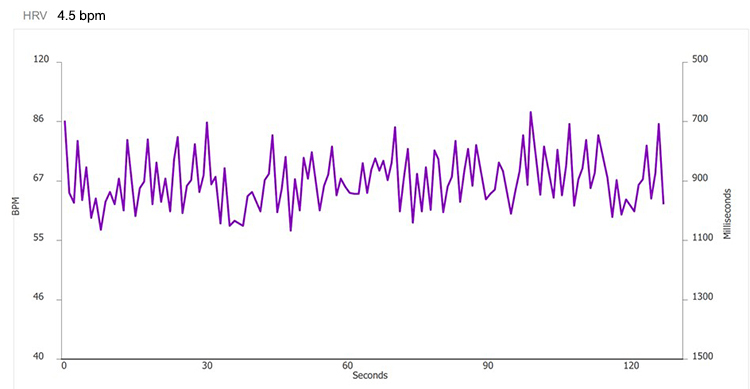
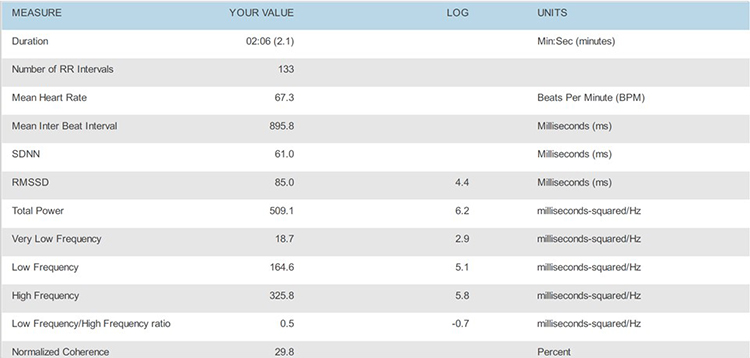
Place the HRV time-domain and frequency-domain values in a table.
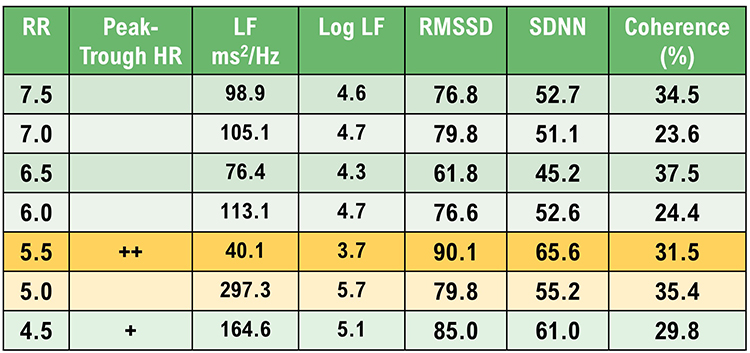
Select the RF using these criteria in descending order: peak-trough HR, largest LF LF normalized power, RMSSD and SDNN, and coherence.
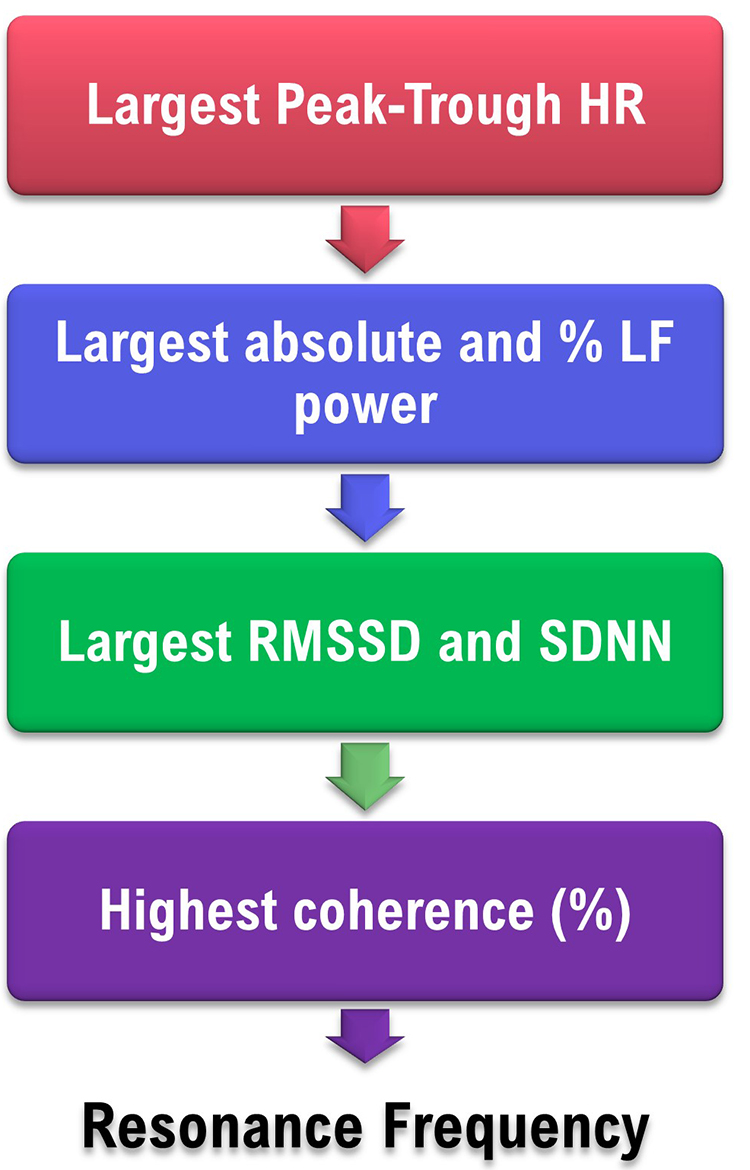
Decision
This client’s RF is either 5.5 or 5.0 bpm based on peak-trough HR, LF power (absolute and %), RMSSD, SDNN, and coherence. The strongest case can be made for 5.5 bpm for its peak-trough HR, RMSSD, and SDNN values.
The choice may come down to your client’s preference. Confirm the RF during the next session by a series of 2-minute trials at the RF, and one-half breath faster and slower.
Can the Coherence Score Identify the RF?
At least for this case, the highest coherence score (37.5%) would have selected one of the least promising frequencies. Breathing at 6.5 bpm was associated with lower peak-trough HR, LF power (absolute and %), RMSSD, and SDNN. Following Lehrer, we encourage RF selection based on a "convergence" of measurements.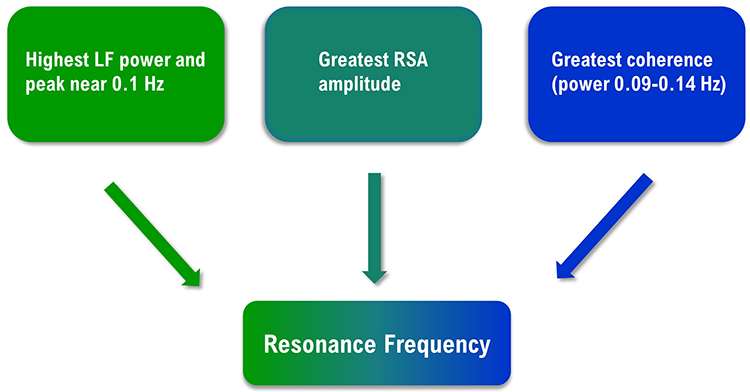
Unanswered Questions
Four significant questions regarding RF assessment require further research. These questions include whether RF training is more effective than 6-bpm slow-paced breathing, the minimum epoch required for valid RF measurements, the Lehrer protocol’s test-retest reliability, and whether rhythmic skeletal muscle tension can replace slow-paced breathing in RF assessment.
Does RF training produce superior outcomes?
While initial studies (Lin et al., 2012; Steffen et al., 2017) found evidence that RF training produces greater systolic blood pressure reductions and more positive mood, a recent meta-analysis (Lehrer et al., 2020a) found non-significant effects on diastolic or systolic blood pressure. Due to the different pathomechanics underlying different disorders, researchers may need to answer this question one disorder at a time (Shaffer & Meehan, 2020).What minimum epoch is required to obtain valid resonance frequency measurements?
Although clinicians may assume that 2-minute recordings achieve acceptable concurrent validity with respect to 5-minute recordings, no peer-reviewed study has demonstrated this result for the most critical RF criteria: heart rate-respiration phase synchrony and HR Max-HR Min.Different epoch lengths may be required for acceptable concurrent validity of related HRV metrics like LF and normalized LF power. Shaffer et al. (2019) evaluated the concurrent validity of these indices in 38 healthy undergraduates. Their concurrent validity criteria included a Pearson’s correlation value = 0.90 and a Bland–Altman limits of agreement allowable difference of ± 5% of the 5-minute value range. Whereas 90-s epochs were sufficient to measure LF power, 180-s records were needed to estimate 5-minute normalized LF power. Researchers should investigate the concurrent validity of all four measures with a larger, more representative sample (Shaffer & Meehan, 2020).
How reliable is RF assessment?
Wally et al. (2011) reported that the RF was stable (r = 0.73. d = 2.14) over a 2-week interval. The authors monitored 21 undergraduate participants using an ECG and respirometer. They required that RR be within 0.25 bpm of the target rate.Capdevila and colleagues (2021) found that the mean group RF was stable from pretest to posttest (6.1 versus 5.9 bpm), as were the group modes (6 versus 6 bpm). However, a granular analysis found that 66.7% of RFs changed from pretest to posttest--although the authors did not specify what constituted a RF change.

The authors failed to use a respirometer to confirm that participants breathed at the target rates and a 1:1 inhalation-to-exhalation (I-E) ratio. Instead, they inferred whether participants followed the paced rhythm by examining each trial's FFT power spectrum. They provided no evidence that this indirect method ensured that participants breathed within 0.25 bpm of the target rate. Additionally, they did not attempt to confirm that their participants breathed at a 1:1 I-E ratio. Without confirmation that participants breathed at the target rates and I-E ratio, inconsistency in breathing could have accounted for individual pretest-posttest RF changes.
The question of test-retest reliability is pivotal for resonance frequency assessment. Why invest an entire session measuring the RF if it changes significantly across training sessions? Researchers should replicate the Wally et al. (2011) findings at a more appropriate 1:2 I-E ratio and a larger and more representative sample.
Could rhythmic skeletal muscle tension replace slow-paced breathing in RF assessment?
Rhythmic skeletal muscle tension (RSMT) can stimulate the baroreflex like resonance frequency breathing and increase LF HRV power (Vaschillo et al., 2011). In this study, participants in a semi-recumbent position rhythmically contracted their hands and feet 3, 6, and 12 times per min. RSMT only produced high-amplitude oscillations in blood pressure, heart rate, and vascular tone at 6 contractions per min (cpm) – a frequency of 0.1 Hz.These findings raise the possibility that clinicians could use RSMT instead of slow-paced breathing to measure the RF and deliver HRV biofeedback training. The RSMT protocol would avoid the challenging requirement that individuals breathe at prolonged rates (e.g., 4.5–6.5 bpm). Before this protocol can be adopted, research will have to prove that it achieves acceptable criterion validity – confirmation that test scores accurately estimate scores of validated measures (Gulliksen, 1987) – with respect to slow-paced breathing and test-retest validity (Shaffer & Meehan, 2020).

What does it mean when the HR tracing peaks before the respirometer tracing during RF assessment?
When the HR tracing (pink) peaks before the respirometer tracing (violet), as in the screens for 4.5 and 5.0 bpm, the client's RR is below their RF. The right screen shows that the HR and respirometer peaks align at 5.5 bpm.
 |
 |
 |
Glossary
baroreflex gain: HR change per 1 mmHg change in BP.
coherence: self-coherence; signal power in the 0.09-0.14 region of the LF band.
frequency-domain measures of HRV: the calculation of the absolute or relative power of the HRV signal within four frequency bands.
high-frequency (HF) band: the HRV frequency range from 0.15-.40 Hz representing the inhibition and activation of the vagus nerve by breathing (RSA).
HR Max-HR Min: a HRV index that calculates the average difference between the highest and lowest HRs during each respiratory cycle.
interbeat interval (IBI): the time interval between the peaks of successive R-spikes (initial upward deflections in the QRS complex). The IBI is also called the NN (normal-to-normal) interval.
low-frequency (LF) band: the HRV frequency range of 0.04-0.15 Hz that may represent the influence of PNS and baroreflex activity (when breathing at resonance frequency).
peak-trough HR: the difference between the fastest and slowest HR in each breathing cycle.
resonance frequency: the frequency at which a system, like the cardiovascular system, can be activated or stimulated.
respiratory sinus arrhythmia (RSA): respiration-driven heart rhythm that contributes to the high frequency (HF) component of heart rate variability. Inhalation inhibits vagal nerve slowing of the heart (increasing HR), while exhalation restores vagal slowing (decreasing HR).
respirometer: a sensor that changes resistance to a current as it expands and contracts during the respiratory cycle.
SD1: the standard deviation of the distance of each point from the y = x-axis that measures short-term HRV.
time-domain measures of HRV: indices like SDNN that measure the degree to which the IBIs between successive heartbeats vary.
very-low-frequency (VLF) band: the HRV frequency range of 0.003-0.04 Hz that may represent temperature regulation, plasma renin fluctuations, endothelial and physical activity influences, and possible intrinsic cardiac, PNS, and SNS contributions.
Test Yourself
Click on the ClassMarker logo to take 10-question tests over this unit without an exam password.

REVIEW FLASHCARDS ON QUIZLET
Click on the Quizlet logo to review our chapter flashcards.

Visit the BioSource Software Website
BCIA offers two HRV Biofeedback Certification paths: Biofeedback and Neurofeedback. For Biofeedback, BioSource Software offers Human Physiology to satisfy BCIA's Human Anatomy & Physiology requirement. For Neurofeedback, BioSource provides Physiological Psychology to satisfy BCIA's Physiological Psychology requirement.
BCIA has accredited each course, and they combine affordable pricing ($150) with industry-leading content.

Assignment
These recordings were from a chronic pain patient who received treatment in an interdisciplinary chronic pain program. Look at the summary screens for pacing at 6.5 and 6.0 breaths per minute. Based on these data, which respiration rate is closer to the client's resonance frequency? Why?
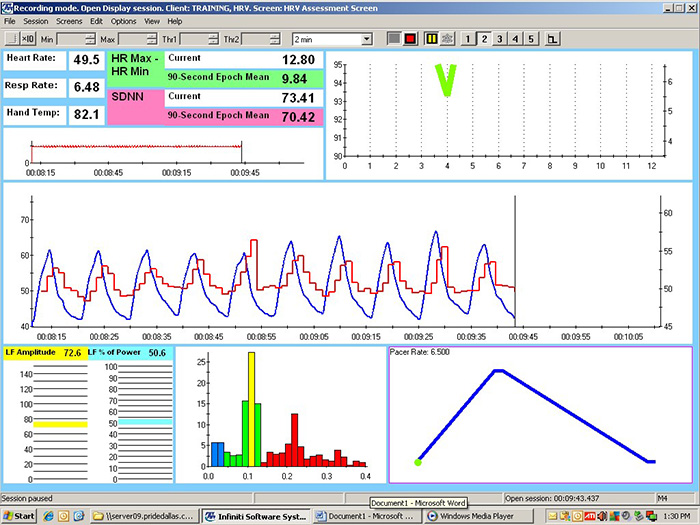
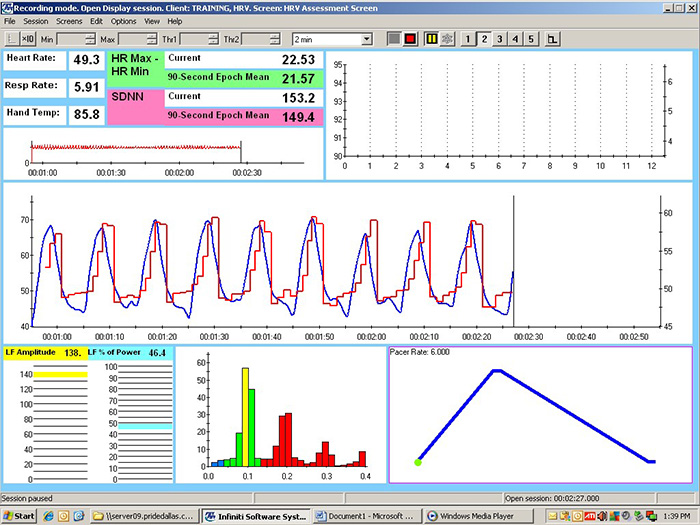
Check the mean respiration rates to confirm that this client breathed at the pacing rates. He did. Examine the values for HR Max - HR Min and LF amplitude. Both were higher at 6.0 than 6.5. Inspect the synchrony of the HR and respirometer tracings. The peaks and valleys of these tracing were more closely aligned at 6.0 than 6.5 breaths per minute. Finally, compare the hand temperatures. His hands were almost 4 degrees F warmer at 6.0 than 6.5. The overall pattern of his measurements argues for training at 6.0 breaths per minute. If the clinic had monitored skin conductance during this session, it might have decreased at the breathing rate closest to his resonance frequency.
References
Allen, J. (2019). Quantifying the delays between multi-site photoplethysmography pulse and electrocardiogram R-R interval changes under slow-paced breathing. Front. Physiol.,10, 1190. https://doi.org/ 10.3389/fphys.2019.01190
Buchheit, M. (2010). Respiratory sinus arrhythmia and pulmonary gas exchange efficiency: Time for a reappraisal. Exp. Physiol., 95, 767. https://doi.org/10.1113/expphysiol.2010.053470
Capdevila, L., Parrado, E., Ramos-Castro, J., Zapata-Lamana, R., & Lalanza, J. F. (2021). Resonance frequency is not always
stable over time and could be
related to the inter-beat interval. Scientific Reports, 11, 8400. https://doi.org/10.1038/s41598-021-87867-8
Cipresso, P., Colombo, D., & Riva, G. (2019). Computational psychometrics using psychophysiological measures for the assessment of acute mental stress. Sensors, 19, 781. https://doi.org/10.3390/s19040781
Fisher, L. R., & Lehrer, P. M. (2022). A method for more accurate determination of resonance frequency of the cardiovascular system, and evaluation of a program to perform It. Applied psychophysiology and biofeedback, 47(1), 17–26. https://doi.org/10.1007/s10484-021-09524-0
Gevirtz, R. N. (2005). Heart rate variability biofeedback in clinical
practice. AAPB Fall workshop.
Giardino, N. D., Lehrer, P. M., & Edelberg, R. (2002). Comparison of finger plethysmograph to ECG in the measurement of heart rate variability. Psychophysiology, 39, 246–253. https://doi.org/10.1111/1469-8986.3920246
Gulliksen, H. (1987). Theory of mental tests. Erlbaum.
Jan, H. Y., Chen, M. F., Fu, T. C., Lin, W. C., Tsai, C. L., & Lin, K. P. (2019). Evaluation of coherence between ECG and PPG derived parameters on heart rate variability and respiration in healthy volunteers with/without controlled breathing. J. Med. Biol. Eng., 39, 783–795. https://doi.org/0.1007/s40846-019-00468-9
Khazan, I. (2019a). Biofeedback and mindfulness in everyday life: Practical solutions for improving your health and performance. W. W. Norton & Company.
Khazan, I. (2019b). A guide to normal values in biofeedback. Physiological recording technology and applications in biofeedback and neurofeedback. In D. Moss & F. Shaffer (Eds.). Association for Applied Psychophysiology and Biofeedback, 2–6.
Khazan, I. Z. (2013). The clinical handbook of biofeedback: A step-by-step guide for training and practice with mindfulness. Wiley-Blackwell.
Lehrer, P., Kaur, K., Sharma, A., Shah, K., Huseby, R., Bhavsar, J., Sgobba, P., & Zhang, Y. (2020a). Heart rate variability biofeedback improves emotional and physical health and performance: A systematic review and meta-analysis. Applied Psychophysiology and Biofeedback, 45, 109–129. https://doi.org/10.1007/s10484-020-09466-z
Lehrer, P., Vaschillo, B., Zucker, T., Graves, J., Katsamanis, M., Aviles, M., & Wamboldt, F. (2013). Protocol for heart rate variability biofeedback training. Biofeedback, 41(3), 98-109. https://doi.org/10.5298/1081-5937-41.3.08
Lehrer, P. M. (2013). Personal communication regarding the test-retest reliability of the resonance frequency in adults.
Lehrer, P. M., & Gevirtz, R. (2014). Heart rate variability: How and why does it work? Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2014.00756
Lehrer, P. M., Vaschillo, E., & Vaschillo, B. (2000). Resonant frequency biofeedback training to increase cardiac variability: Rationale and manual for training. Applied Psychophysiology and Biofeedback, 25(3),
177-191. https://doi.org/10.5298/1081-5937-41.3.08
Lin, G., Xiang, Q., Fu, X., Wang, S., Wang, S., Chen, S., . . . Wang, T. (2012). Heart rate variability biofeedback decreases blood pressure in prehypertensive subjects by improving autonomic function and baroreflex. J. Altern. Complement. Med., 18, 143–152. https://doi.org/10.1089/acm.2010.0607
Meehan, Z., Muesenfechter, N., Gravett, N., Watson, T., Smith, A., Shearman, S., . . . Shaffer, F. (2017). A 1:2 inhalation-to-exhalation ratio does not increase heart rate variability during 6-bpm breathing [Abstract]. Applied Psychophysiology and Biofeedback, 45, 110–111. https://doi.org/10.1007/s10484-018-9390-8
Peper, E., Gibney, K. H., Tylova, H., Harvey, R., & Combatalade, D. (2008). Biofeedback mastery: An experiential teaching and self-training manual. Association for Applied Psychophysiology and Biofeedback.
Schafer, A., & Vagedes, J. (2013). How accurate is pulse rate variability as an estimate of heart rate variability? A review on studies comparing photoplethysmographic technology with an electrocardiogram. Int. J. Cardiol., 166, 15–29. https://doi.org/10.1016/j.ijcard.2012.03.119
Shaffer, F., & Combatalade, D. (2013). Don’t add or miss a beat: a guide to cleaner heart rate variability recordings. Biofeedback, 41, 121–130. https://doi.org/10.5298/1081-5937-41.3.04
Shaffer, F., & Meehan, Z. M. (2020). A practical guide to resonance frequency assessment for heart rate variability biofeedback. Frontiers in Neuroscience. https://doi.org/10.3389/fnins.2020.570400
Shaffer, F., & Moss, D. (2019). Biofeedback. Brain and heart dynamics. In D. Bugada, V. Bellini, E. G. Bignami, & L. F. Lorini (Eds.). Springer, 1–15.
Steffen, P. R., Austin, T., DeBarros, A., & Brown, T. (2017). The impact of resonance frequency breathing on measures of heart rate variability, blood pressure, and mood. Front. Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
Strauss-Blasche, G., Moser, M., Voica, M., McLeod, D., Klammer, N., & Marktl, W. (2000). Relative timing of inspiration and expiration affects respiratory sinus arrhythmia. Clin. Exp. Pharmacol. Physiol., 27, 601–606. https://doi.org/10.1046/j.1440-1681.2000.03306.x
Vaschillo, E., Lehrer, P., Rishe, N., & Konstantinov, M. (2002). Heart rate variability biofeedback as a method for assessing baroreflex function: A preliminary study of resonance in the cardiovascular system. Applied Psychophysiology and Biofeedback, 27(1), 1-27. https://doi.org/10.1023/a:1014587304314
Van Diest, I., Verstappen, K., Aubert, A. E., Widjaja, D., Vansteenwegen, D., & Vlemincx, E. (2014). Inhalation/exhalation ratio modulates the effect of slow breathing on heart rate variability and relaxation. Applied Psychophysiology and Biofeedback, 39, 171–180. https://doi.org/10.1007/s10484-014-9253-x
Vaschillo, E. G., Vaschillo, B., & Lehrer, P. M. (2004). Heartbeat synchronizes with respiratory rhythm only under specific circumstances. Chest, 126, 1385–1386. https://doi.org/10.1016/S0012-3692(15)31329-5
Vaschillo, E. G., Vaschillo, B., Pandina, R. J., & Bates, M. E. (2011). Resonances in the cardiovascular system caused by rhythmical muscle tension. Psychophysiology, 48, 927-936. https://dx.doi.org/10.1111%2Fj.1469-8986.2010.01156.x
Wally, C., Korenfeld, I., Brooks, K., Carrell, D., Lau, D., Peterson, J., Schafer, M., Truitt, A., Fuller, J., Westermann-Long, A., & Korenfeld, D. (2011). Resonance frequency measurements are reliable [Abstract]. Poster presented at the meeting of the Association for Applied Psychophysiology and Biofeedback, New Orleans, Louisiana.
Weinschenk, S. W., Beise, R. D., & Lorenz, J. (2016). Heart rate variability (HRV) in deep breathing tests and 5-min short-term recordings: Agreement of ear photoplethysmography with ECG measurements, in 343 subjects. Eur. J. Appl. Physiol., 116, 1527–1535. https://doi.org/10.1007/s00421-016-3401-3
Zerr, C., Kane, A., Vodopest, T., Allen, J., Hannan, J., Fabbri, M., . . . Shaffer, F. (2015). Does inhalation-to-exhalation ratio matter in heart rate variability biofeedback? [Abstract]. Applied Psychophysiology and
Biofeedback, 40(2), 135. https://doi.org/10.1007/s10484-015-9282-0
