Electrocardiogram (ECG) Instrumentation
The electrocardiogram provides the most accurate measurement of heart rate and heart rate variability. Clinicians need to recognize clean signals, identify significant artifact sources, and understand how to prevent them. A tracking test helps ensure that your data acquisition system faithfully displays changes in client HRV.

BCIA Blueprint Coverage
This unit addresses III. HRV Instrumentation: B. The electrocardiogram (ECG/EKG).
Professionals completing this unit will be able to discuss electrocardiogram:
A. Source
B. ECG sensor
C. Signal
D. Placements
E. Tracking Test
F. Artifacts

This unit covers the Source of the ECG, ECG Sensors, ECG Signal, Sampling Rate, ECG Sensor Placement, ECG Artifacts, and Tracking Tests.
Please click on the podcast icon below to hear a full-length lecture.

Source of the ECG Signal
In a healthy heart, the SA node initiates each cardiac cycle by spontaneously depolarizing its autorhythmic fibers. The SA node's firing of 60-100 action potentials per minute usually prevents slower parts of the conduction system and myocardium (heart muscle) from generating competing potentials. Graphic © Alila Medical Media/Shutterstock.com.
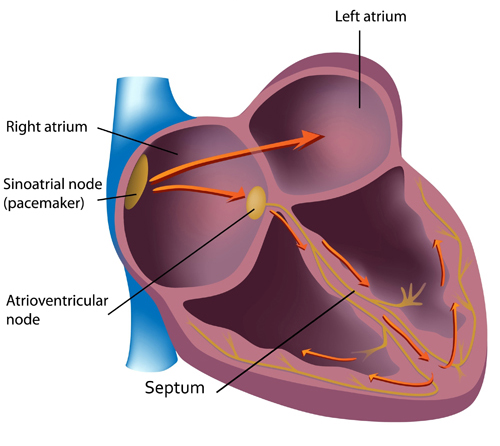
The SA node fires an impulse that travels through the atria to the AV node in about 0.03 seconds and causes the AV node to fire. The P wave of the ECG is produced as contractile fibers in the atria depolarize. The P wave culminates in the contraction of the atria (atrial systole). Animation © 2010 Scholarpedia.
ECG Sensors
Three- or four-lead electrode assemblies are sufficient to record the ECG signal. There is no universal color-coding system for ECG electrodes (Lehrer, 2018b). ECG sensors can be identical to EMG sensors. Standard lead cables have snap buttons onto which the electrodes are affixed. A MindMedia EXG sensor is shown below.

Dry or gelled electrodes can be used. Pre-gelled disposable ECG electrodes save preparation time and reduce the risk of infection.

Skin Preparation
Prepare the skin by rubbing the area where the electrodes will be applied with an alcohol wipe. Cleaning the skin of oil and dirt helps reduce impedance, which is the opposition to AC flow. You may need to shave the chest and abdomen if body hair prevents satisfactory electrode contact with the skin for men. The multi-lead configuration shown below is used for diagnostic ECGs, not HRV biofeedback. Graphic © Bork/Shutterstock.com.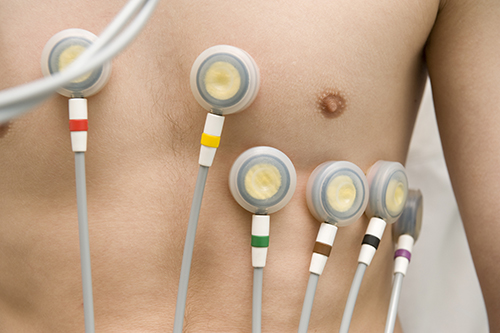
ECG Signal
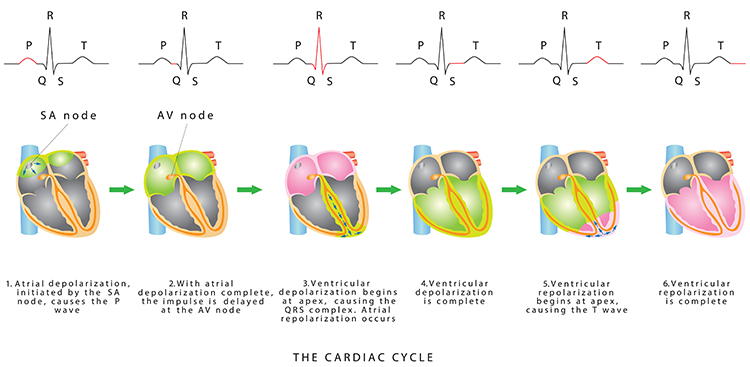
The signal from the SA node rapidly spreads through the atrioventricular (AV) bundle reaching the top of the septum. Descending right and left bundle branches conduct the action potential over the ventricles about 0.2 seconds after the appearance of the P wave.
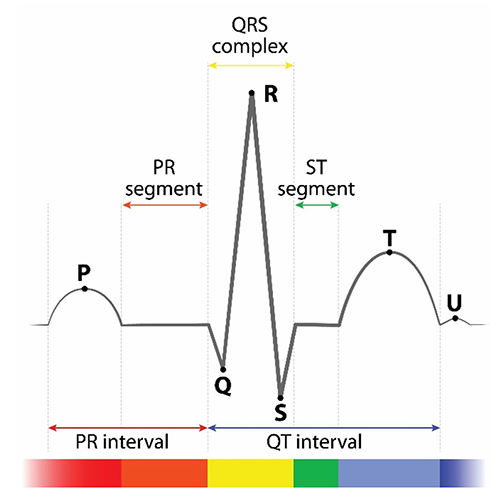
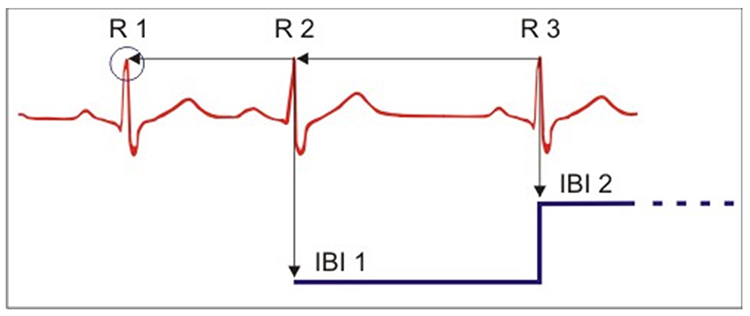
Conduction myofibers extend from the bundle branches into the myocardium, depolarizing contractile fibers in the ventricles (lower chambers). Ventricular depolarization generates the QRS complex. The software uses the R-spike (depicted below at 3) to detect a heartbeat and measure the IBI.
The ventricles contract (ventricular systole) soon after the emergence of the QRS complex. Their contraction continues through the S-T segment. Ventricular contractile fiber depolarization generates the T wave about 0.4 seconds following the P wave. The ventricles relax (ventricular diastole) 0.6 seconds after the P wave begins (Tortora & Derrickson, 2021).
Check out the YouTube video 15 Second EKG. Graphic © lotan/Shutterstock.com.
Sampling Rate
The Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996) recommended an ECG sampling rate of at least 250-500 Hz without interpolation. Laborde et al. (2017) advised a minimum 125-Hz rate for research. Where RSA amplitude is low, they suggested a minimum 500-Hz rate.
Placements
Six standard ECG electrode placements can be used. These include the wrist, wrist-to-ankle, forearm, lower torso, and chest (upper chest/xiphoid; heart level). These placements differ in vulnerability to skeletal muscle (EMG) or movement artifact, speed of application, and degree of client comfort.
Listen to a mini-lecture on Six ECG Placements © BioSource Software LLC.
Wrist Placement
A wrist placement requires electrode straps instead of adhesive electrodes. One strap is used to attach an active electrode to the right wrist and the other to attach the reference and second active electrode to the left wrist. While the easiest, most socially comfortable, and quickest ECG electrode placement, it is highly vulnerable to arm EMG and movement artifacts.
Wrist-to-Ankle Placement
Place the active (+) electrodes on the left wrist and ankle and the reference (-) electrode on the right wrist.
The right arm to left leg placement often accentuates the R-spike in individuals with large T-waves and is less invasive than chest or lower torso placements. This placement is more vulnerable to movement artifacts than the chest or lower torso placement (Lehrer, 2018). Graphic © Designua/Shutterstock.com.
Forearm Placement
A forearm placement locates an active electrode on the right forearm and the reference and secondactive electrodes on the left forearm. Select an area with minimal or no hair. This placement is more vulnerable to contamination by arm and chest EMG and movement artifacts.
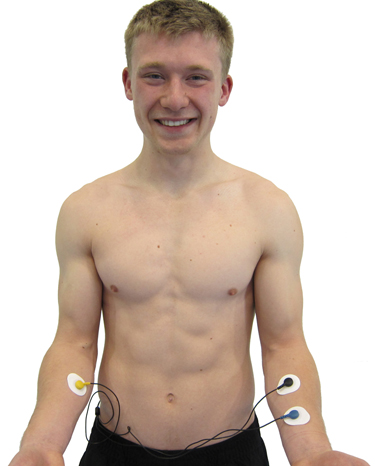
Lower Torso Placement
A lower torso placement suggested by Peper (2010) centers the reference electrode over the angle of the sternum and the active electrodes about 5 centimeters above the navel and 10 centimeters to the left and right of the midline. This placement provides an alternative for clients who are uncomfortable exposing their chests (they can lift their blouse or shirt) and is less vulnerable to arm EMG artifact and movement artifacts..jpg)
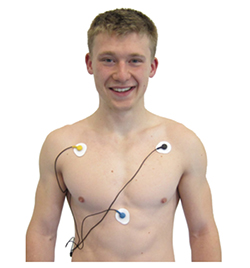
Chest Placement
A chest placement locates active and reference electrodes over the right and left coracoid processes, respectively, and a second active electrode over the xiphoid process. This placement reduces the risk of arm muscle artifact but exposes the chest area, which can be uncomfortable for female clients (Shaffer & Combatalade, 2013).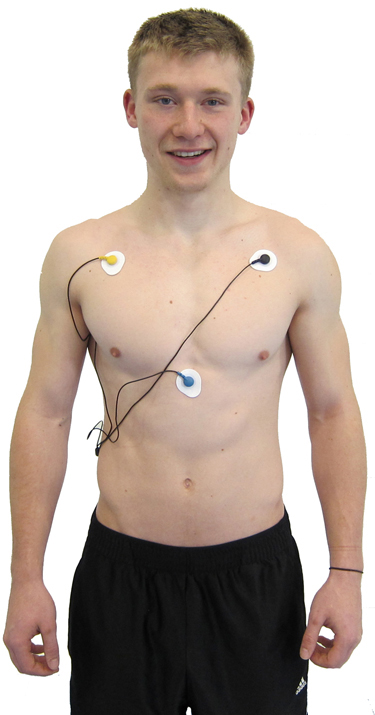
An alternative chest placement locates all three electrodes in a row at heart level. This sensor arrangement can detect the largest-amplitude R-spikes (Lehrer, 2018b).
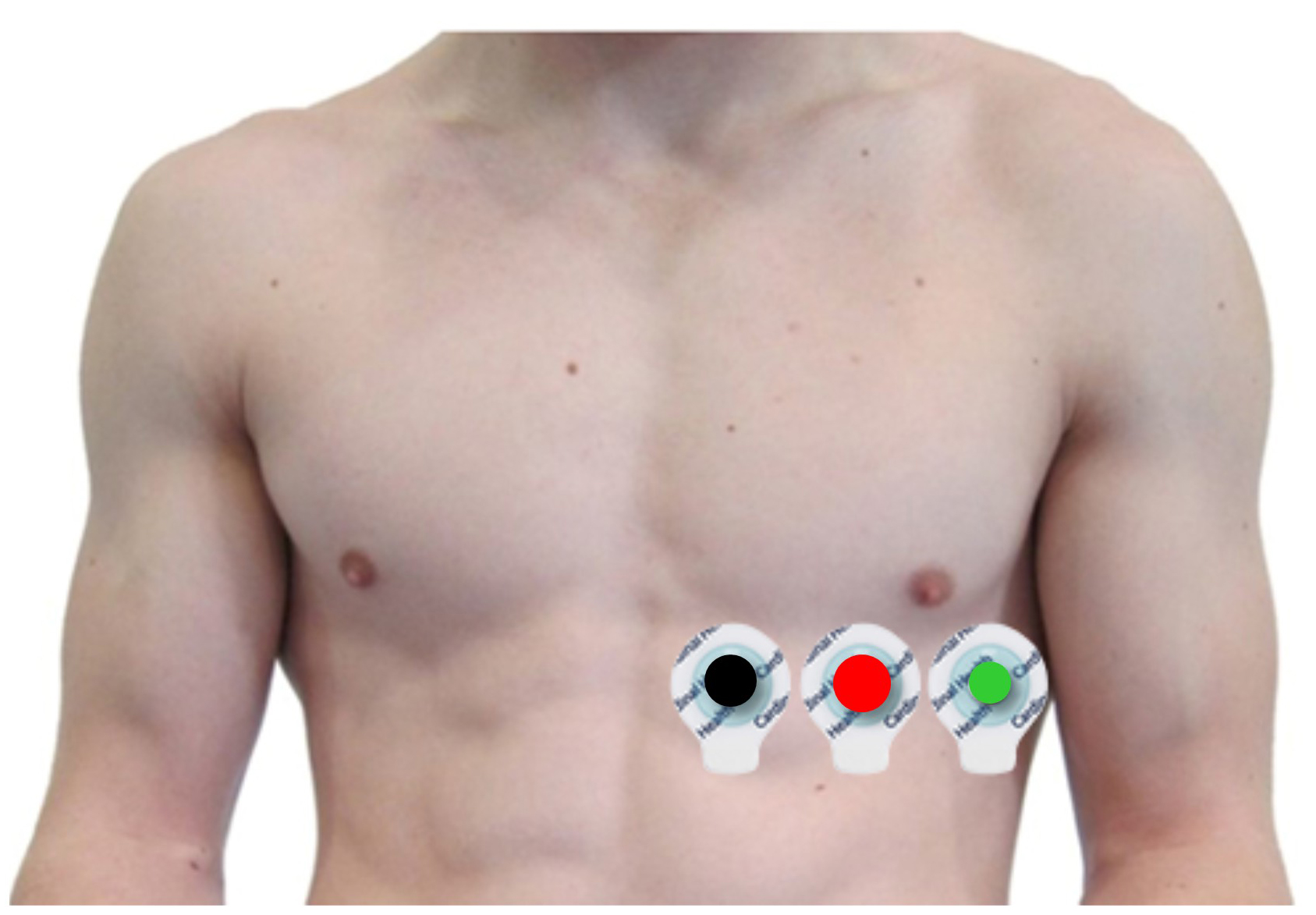
The Lief Therapeutics sensor uses this placement. Graphic © Lief Therapeutics.

Placement Summary
Wrist or forearm placements offer greater client comfort and quicker application speeds where EMG and movement artifacts don't contaminate your recordings. When these artifacts are present, the lower torso placement may be best for research. Sensor placement on the upper chest and abdomen requires client/participant education and written informed consent.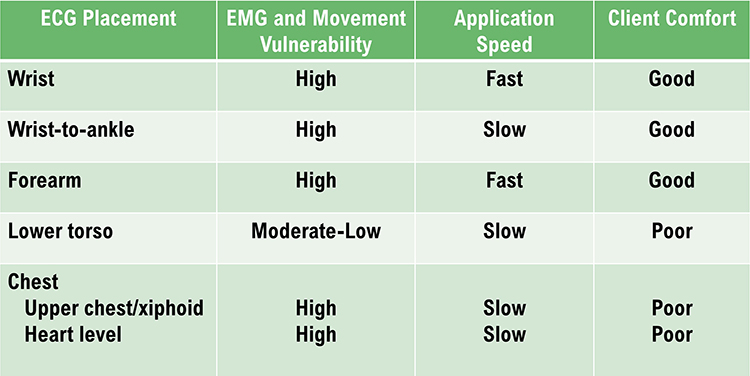
Review the ECG
Click on the graphic below to review the ECG Quizlet set by Stephanie Verbeek.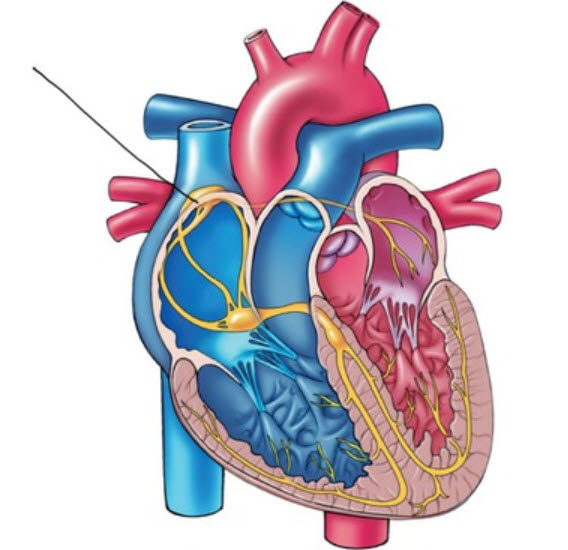
ECG Artifacts
ECG recording is vulnerable to diverse artifacts. Missing or extra beats, 50/60Hz noise, EMG, respiration, movement, DC offset, electromagnetic (EMI), and electrode polarity produce the most important artifacts.
Missed and Extra Beats
HRV software determines the interbeat interval (IBI) by detecting adjacent beats and measuring the time between R-spikes.Listen to a mini-lecture on Missed and Extra Beats © BioSource Software LLC. Graphic © arka38/Shutterstock.com.
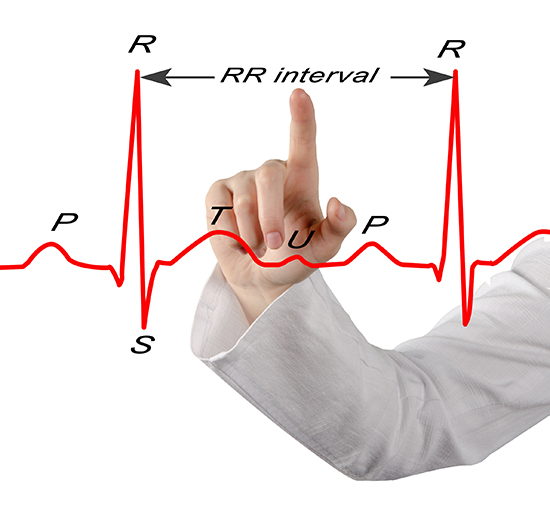
After detecting the first beat, the software starts counting and calculates the first IBI in milliseconds. This process is repeated until the end of the epoch or data collection period. Graphic courtesy of Dick Gevirtz.
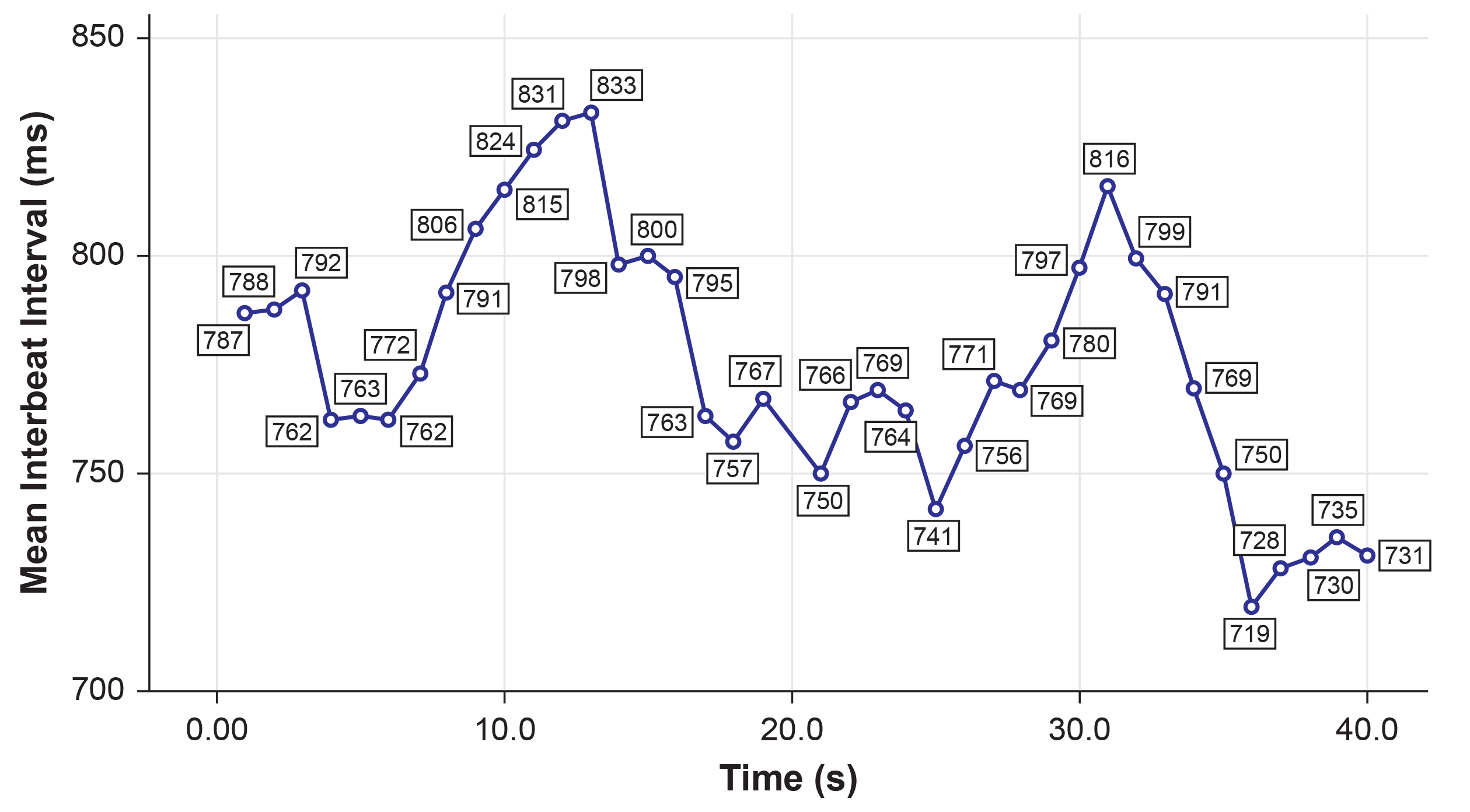
IBI measurements are the basis of statistical calculations of time-domain (pNN50, RMSSD, and SDNN), frequency-domain (VLF, LF, and HF), and nonlinear measurements.
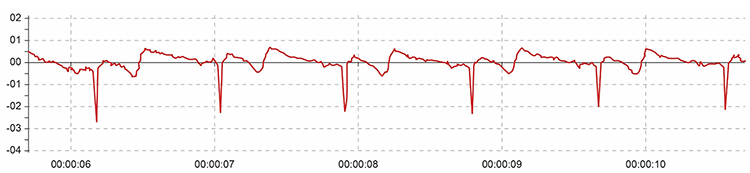
When distortion prevents software from detecting a heartbeat, this results in a missed beat and a prolonged interbeat interval (IBI) calculation. On the graph below, a missed beat generated the circled IBI (1500 ms).
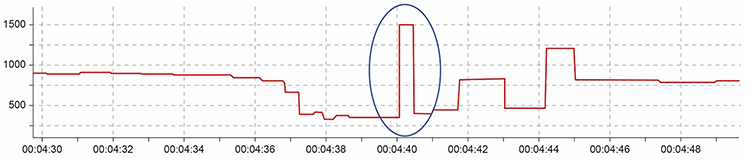
Conversely, when distortion causes the software to detect an extra beat, this produces an artifactually short interbeat interval (IBI). As emphasized earlier, missed and extra beats also affect PPG recording (Elgendi, 2012).
Watch for These Artifacts
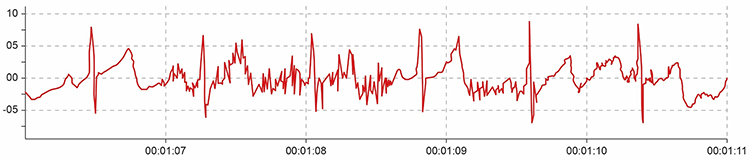
Inspect the raw ECG signal for line interference, EMG, movement, DC offset, electromagnetic interference, radiofrequency, and polarity artifacts.
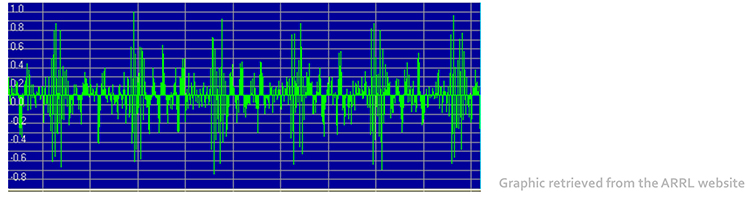
Line Interference (50/60 Hz) Artifact
Line interference artifact is the most frequent source of ECG signal contamination.Listen to a mini-lecture on ECG Line Interference Artifact © BioSource Software LLC.
It doesn’t affect the BVP signal because it is based on back-scattered or transmitted infrared light. Primary sources of this artifact include computers, computer monitors, fluorescent lights, and power outlets. The line interference artifact looks fuzzy because high-frequency fluctuations are superimposed on the signal (Shaffer & Combatalade, 2013).


Clinical Tips to Minimize Line Interference (50/60Hz) Artifact
1. Use a 50/60Hz notch filter.
2. Place the encoder box 3 feet (1 meter) from electronic equipment.
3. Remove unused sensor cables from the encoder box.
4. Carefully prepare the skin.
5. Apply pre-gelled electrodes to achieve low and balanced impedances (10 Kohms/5 Kohms).
6. Examine the raw signal for artifacts.
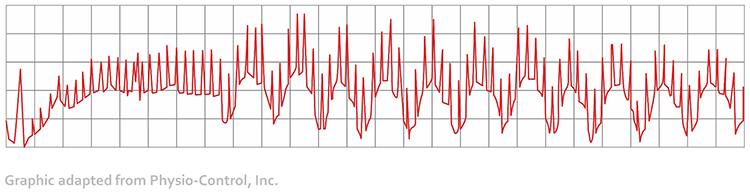
EMG Artifact
Frequencies generated by the depolarization of skeletal muscles overlap with the ECG spectrum and produce EMG artifacts.Listen to a mini-lecture on ECG EMG Artifact © BioSource Software LLC.
The surface EMG ranges from 1-1,000 Hz (Stern, Ray, & Quigley, 2001), while the ECG extends from 0.1-1,000 Hz (Langner & Geselowitz, 1960). Muscle action potentials from large muscle groups travel to ECG sensors via volume conduction (Shaffer & Neblett, 2010).
The contraction of arm muscles can cause the software to "see" many extra beats and calculate shorter IBIs (Shaffer & Combatalade, 2013).
While EMG artifact affects ECG recordings, it does not contaminate the BVP signal since we detect it using infrared light.
Clinical Tips to Minimize EMG Artifacts1. Use chest or lower rib placements instead of forearm or wrist placements.
2. Instruct your client to sit in a relaxed position and restrict movement, and verify compliance.
3. Examine the raw signal for artifacts.
Movement Artifact
Client movement can pull the electrode cable so that the electrode partially (or completely) loses contact with the skin.Listen to a mini-lecture on ECG Movement Artifact © BioSource Software LLC.
Movement artifact consists of high-amplitude signal fluctuations that cause the software to "see“ many extra beats and calculate shorter IBIs as with EMG artifact.
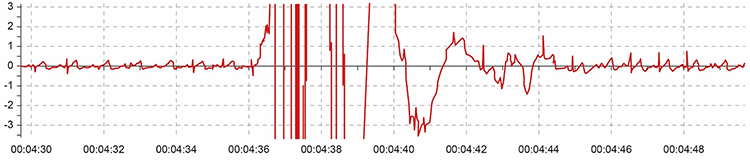
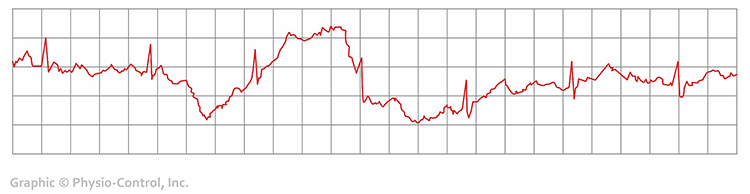
Below is a BioGraph ® Infiniti ECG display of movement artifact. The ECG (also called EKG) waveform abruptly shifts upward after the sixth heartbeat and then returns to normal. You can enlarge the video by clicking on the bracket icon at the bottom right of the screen. When finished, click on the ESC key.
Clinical Tips to Minimize Movement Artifact
1. Firmly tape sensor leads to client clothing for strain relief to restrict movement.
2. Use a lower torso placement.
3. Use pre-gelled electrodes to ensure strong skin-electrode contact.
4. Provide instructions to sit in a relaxed position and restrict movement, and confirm compliance.
5. Examine the raw signal for artifacts.
Respiration Artifact
Respiration artifacts can result from dried gel and inadequate skin preparation.Listen to a mini-lecture on ECG Respiration Artifact © BioSource Software LLC.
Clinical Tips to Control Respiration Artifact
1. Abrade the skin after cleaning with an alcohol wipe.
2. Use pre-gelled electrodes to ensure strong skin-electrode contact.
Direct Current (DC) Offset Artifact
DC offset artifact occurs when the skin-electrode impedances of the three ECG electrodes differ due to poor skin-electrode contact.Listen to a mini-lecture on ECG Direct Current Offset Artifact © BioSource Software LLC.
The ECG signal may drift up or down, causing extra beats or missed beats.

Clinical Tips to Minimize DC Offset Artifact
1. Clean the skin using an alcohol wipe.
2. Use fresh electrodes with sufficient gel.
3. Examine the raw signal for artifacts.
Electromagnetic Interference (EMI) Artifacts
Electromagnetic interference (EMI) artifacts are generated by cell phones when they are less than 6 ft (2 m) from ECG sensors or encoder boxes (Peper & Lin, 2010).Listen to a mini-lecture on ECG Electromagnetic Interference Artifacts © BioSource Software LLC.
Computer monitors and television screens are sources of EMI artifacts. These are also called radiofrequency (RF) artifacts. High-frequency energy expands outward from a monitor like a cone (Montgomery, 2004).
Also, watch out for audiovisual systems and high-voltage equipment like centrifuges, elevators, and x-ray machines (Lehrer, 2018b).
Clinical Tips to Minimize Electromagnetic Interference Artifacts
1. Ensure that all cell phones are turned off.

2. Maintain an adequate distance from high-voltage equipment (Lehrer, 2018b).
3. Position an encoder box or separate instruments behind or to the monitor's side.
4. Place the client no closer than 2-3 feet from the monitor (Montgomery, 2004).
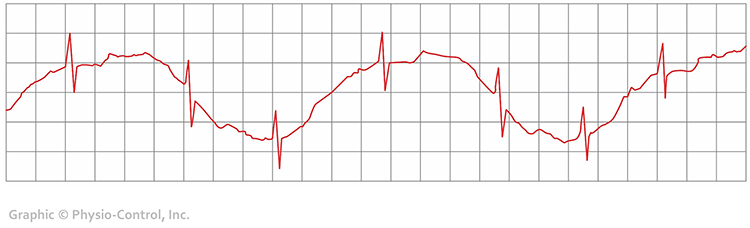
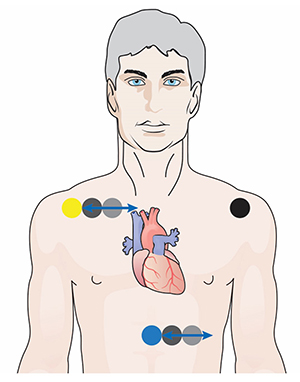
Polarity Artifact
Polarity artifact occurs when the active electrodes (yellow and blue for Thought Technology) are misaligned with respect to the heart’s axis.Listen to a mini-lecture on ECG Polarity Artifact © BioSource Software LLC.
A low-amplitude downward-oriented R-spike can cause the software to miss beats and lengthen the IBI.
Software packages like J & J Engineering’s Physiolab automatically correct for polarity artifact (Lehrer, 2018b).
Clinical Tips to Minimize Polarity Artifact
1. Locate active electrodes on the right shoulder and over the xiphoid process (extension of the lower sternum).
2. Laterally adjust electrode position to increase R-spike amplitude.
3. The best location may require experimentation.
Tracking Test
Using a respirometer, you can determine whether the ECG signal responds to your client's breathing by observing whether instantaneous HR speeds during inhalation and slows during exhalation (gray line) (Nederend et al., 2016).
Listen to a mini-lecture on the ECG Tracking Test © BioSource Software LLC.
The BioGraph ® Infiniti display below shows that instantaneous HR (pink) speeds and slows as the abdominal strain gauge (purple) rhythmically expands and contracts. You can enlarge the video by clicking on the bracket icon at the bottom right of the screen. When finished, click on the ESC key.
ECG and Respiration Demonstration
Dr. Inna Khazan demonstrates ECG and respiration recording, artifacts, and a tracking test © Association for Applied Psychophysiology and Biofeedback. You can enlarge the video by clicking on the bracket icon at the bottom right of the screen. When finished, click on the ESC key.

Which ECG placement would you recommend for HRV training? Why?
Select a wrist or forearm placement when client comfort and preparation time are your primary concerns. Consider Erik Peper's lower torso placement if these placements produce unacceptable movement artifacts.
Glossary
active electrodes: negative and positive ECG electrodes that may be placed on the right upper chest and below the sternum, above the palmar surface of the right and left wrists, or above the palmar surface of the right wrist and the left knee.
artifact: measurement errors in calculating the interbeat interval.
DC offset artifact: an ECG artifact that lengthens the IBI when differences in skin-electrode impedance produce signal drift causing the software to miss beats.
electromagnetic interference (EMI) artifact: an ECG artifact generated when cell phones transmit an artifactual voltage.
EMG artifact: an ECG artifact that shortens the IBI when signal contamination by the EMG causes the software to detect nonexistent beats.
extra beats: an ECG artifact that shortens the IBI when signal distortion causes the software to detect nonexistent beats.
heart rate: the number of heartbeats per minute, also called stroke rate.
heart rate variability (HRV): the beat-to-beat changes in heart rate, including changes in the RR intervals between consecutive heartbeats.
HR Max – HR Min: an index of heart rate variability that calculates the difference between the highest and lowest heart rates during each respiratory cycle.
interbeat interval (IBI): the time interval between the peaks of successive R-spikes (initial upward deflections in the QRS complex). The IBI is also called the NN (normal-to-normal) interval.
line interference artifact: ECG and PPG artifact when 50/60Hz contamination of signals causes the software to detect nonexistent beats and shorten the IBI.
missed beats: ECG artifact that lengthens the IBI when signal distortion causes the software to overlook a beat and use the next good beat.
movement artifact: ECG and PPG artifact that shortens the IBI when signal distortion from movement causes the software to detect nonexistent beats.
pNN50: the percentage of adjacent NN intervals that differ by more than 50 milliseconds.
polarity artifact: an ECG artifact when reversed electrode placement inverts the direction of the R-spike and causes the software to miss beats and lengthen the IBI.
reference electrode: ground ECG electrode that may be placed on the left upper chest, below the palmar aspect of the left elbow, or above the palmar aspect of the left wrist.
resolution: degree of detail in a biofeedback display (0.1 mV) or the number of voltage levels that an A/D converter can discriminate (16 bits or discrimination among 65,536 voltage levels).
respiratory sinus arrhythmia (RSA): respiration-driven heart rhythm that contributes to the high frequency (HF) component of heart rate variability. Inhalation inhibits vagal nerve slowing of the heart (increasing heart rate), while exhalation restores vagal slowing (decreasing heart rate).
RMSSD: the square root of the mean squared difference of adjacent NN intervals.
SDANN: the standard deviation of the average 5-minute NN intervals that estimates heart rate changes produced by cycles longer than 5 minutes.
SDNN: the standard deviation of the interbeat interval measured in milliseconds, which predicts morbidity and mortality.
SDRR: the standard deviation of the interbeat interval for all sinus beats measured in milliseconds, which predicts morbidity and mortality.
tracking test: checks of whether the biofeedback display mirrors client behavior. Instantaneous heart rate detected by ECG sensors should speed and slow as the client inhales and exhales.
Test Yourself
Click on the ClassMarker logo to take 10-question tests over this unit without an exam password.

REVIEW FLASHCARDS ON QUIZLET
Click on the Quizlet logo to review our chapter flashcards.

Visit the BioSource Software Website
BCIA offers two HRV Biofeedback Certification paths: Biofeedback and Neurofeedback. For Biofeedback, BioSource Software offers Human Physiology to satisfy BCIA's Human Anatomy & Physiology requirement. For Neurofeedback, BioSource provides Physiological Psychology to satisfy BCIA's Physiological Psychology requirement.
BCIA has accredited each course, and they combine affordable pricing ($150) with industry-leading content.

Essential Skills
ECG
1. Explain the ECG signal and biofeedback to a client.
2. Explain ECG sensor attachment to a client and obtain permission to monitor her.
3. Explain how to select a placement site and demonstrate how to attach ECG sensors to minimize movement artifacts.
4. Demonstrate skin preparation.
5. Perform a tracking test by asking your client to inhale slowly and then exhale as you watch the change in heart rate.
6. Identify movement artifact in the raw ECG signal and explain how to control movement, and remove this artifact from the raw data.
7. Explain the major measures of heart rate variability, including HR Max - HR Min, pNN50, SDNN, and SDRR.
8. Explain why we train clients to increase power in the low-frequency band of the ECG and how breathing at 5-7 breaths per minute helps them accomplish this.
9. Demonstrate how to instruct a client to utilize a feedback display.
10. Describe strategies to help clients increase their heart rate variability.
11. Demonstrate an HRV biofeedback training session, including record keeping, goal setting, site selection, baseline measurement, display and threshold setting, coaching, and debriefing at the end of the session.
12. Demonstrate how to select and assign a practice assignment based on training session results.
13. Evaluate and summarize client progress during a training session.
Assignment
What is wrong with the heart rate signal shown below? What problem could this cause?

The ECG waveform is inverted, with the R-spike pointing downward. While this wasn't a problem for this client, low-amplitude R-spikes could confuse the software algorithm that detects each interbeat interval (IBI), resulting in missed beats and lengthened IBIs. The clinician should reposition the active sensors with respect to the heart's axis to correct R-spike orientation.
Acknowledgment
This unit draws heavily on graphics published in Didier Combatalade’s Basics of Heart Rate Variability Applied to Psychophysiology, published by Thought Technology Ltd. Didier is the Director of Clinical Interface at Thought Technology Ltd and is a gifted educator and writer, and generous colleague.

References
Andreassi, J. L. (2000). Psychophysiology: Human behavior and physiological response. Lawrence Erlbaum and Associates, Inc.
Berntson, G. G., Quigley, K. S., & Lozano, D. (2007). Cardiovascular psychophysiology. In J. T. Cacioppo, L. G. Tassinary, & G. G. Berntson (Eds.). Handbook of psychophysiology (3rd ed.). Cambridge University Press.
Combatalade, D. (2010). Basics of heart rate variability applied to psychophysiology. Thought Technology Ltd.
Combatalade, D. (2013). CardioPro Infiniti: HRV analysis module for BioGraph Infiniti. Thought Technology Ltd.
Gevirtz, R. N. (2011). Cardio-respiratory psychophysiology: Gateway to mind-body medicine. BFE conference workshop.
Laborde, S., Mosley, E., & Thayer, J. F. (2017). Heart rate variability and cardiac vagal tone in psychophysiological research -- Recommendations for experiment planning, data analysis, and data reporting. Frontiers in Psychology, 8, 213. https://doi.org/10.3389/fpsyg.2017.00213
Lehrer, P. M. (2007). Biofeedback training to increase heart rate variability. In P. M. Lehrer, R. M. Woolfolk, & W. E. Sime (Eds.). Principles and practice of stress management (3rd ed.). The Guilford Press.
Lehrer, P. M. (2012). Personal communication.
Lehrer, P. M., Vaschillo, E., & Vaschillo, B. (2000). Resonant frequency biofeedback training to increase cardiac variability: Rationale and manual for training. Applied Psychophysiology and Biofeedback, 25(3), 177-191. https://doi.org/10.1023/a:1009554825745
Moss, D. (2004). Heart rate variability (HRV) biofeedback. Psychophysiology Today, 1, 4-11.
Nunan, D., Sandercock, G. R. H., & Brodie, D. A. (2010). A quantitative systematic review of normal values for short-term heart rate variability in healthy adults. Pacing and Clinical Electrophysiology, 33(11), 1407-1417. https://doi.org/10.1111/j.1540-8159.2010.02841.x
Shaffer, F., & Combatalade, D. C. (2013). Don't add or miss a beat: A guide to cleaner heart rate variability recordings. Biofeedback, 41(3), 121-130. https://doi.org/10.5298/1081-5937-41.3.04
Shaffer, F., & Neblett, R. (2010, Summer). Practical anatomy and physiology: The skeletal muscle system. Biofeedback, 38(2) 47-51. https://doi.org/10.5298/1081-5937-38.2.47
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996). Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Circulation, 93, 1043-1065. PMID: 8598068
