As a movie audience watches a frightening film, hearts race, palms sweat, pupils dilate, and neck and shoulder muscles brace.
Yet, no one has been grabbed by the throat. Psychological activity affects the body. Conversely,
physiological changes affect psychological activity. Graphic © G-Stock Studio/ Shutterstock.com.

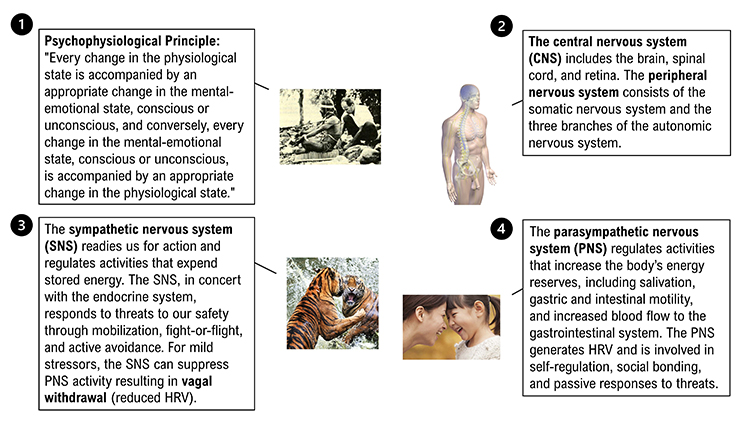
This powerful idea is Green and
Green's
psychophysiological principle.

Listen to a mini-lecture on Psychophysiology © BioSource Software LLC.
Psychophysiology studies the interrelationship between psychological and
physiological processes. Andreassi (2007) wrote:
"Psychophysiology is the study of relations between psychological manipulations and resulting physiological
responses, measured in the living organisms, to promote understanding of the relation between mental and bodily
processes." (p. 2) The interrelationship between psychological and physiological processes is dynamic and
bidirectional.

Biofeedback practitioners study the basic principles of psychophysiology to
understand disease processes and health and how clinical interventions
achieve their results.
The
idiographic approach, which emphasizes
individual differences, is critical to biofeedback practice. Each
client's response to stressors is unique, specific, and often complex.
To effectively treat your client, you need to discover your client's characteristic responses to stressors during a psychophysiological profile administered during the assessment stage of treatment. For example, if hand temperature falls and respiration rate increases during math and visual imagery stressors, you might consider training your client to maintain hand temperature around 90
o
F (32.2
o C) while breathing under 7 breaths-per-minute. This approach may be
superior to using a standard treatment
protocol that disregards your client's unique response pattern or
response stereotypy.
Graphic © Chris Schmidt/ iStockphoto.com.

This unit will challenge the simplistic belief that the sympathetic division fight-or-flight response is our only means of responding to stressors. The parasympathetic branch expands our response options through immobilization, feigning death, passive avoidance, and shutdown, or social engagement supported by the release of the hormone oxytocin. Graphic © Piotr Marcinski/Shutterstock.com.

BCIA Blueprint Coverage
This unit complements the BCIA HRV Biofeedback Blueprint.

This unit covers the Psychophysiological Principle, Homeostasis, Autonomic Balance, Psychophysiological Measurements, Orienting and Defensive Responses, Activation and Habituation, situational Specificity, Law of Initial Values (LIV), Generalization of Biofeedback Training, and the Placebo Effect.
Please click on the podcast icon below to hear a full-length lecture.

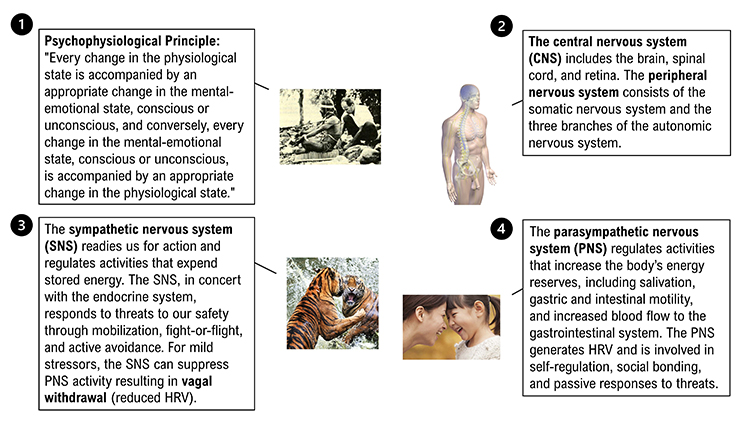
Psychophysiological Principle
Green, Green, and Walters' (1970)
psychophysiological
principle was revolutionary because it proposed a bidirectional relationship between physiological and
psychological functioning:
Every change in the physiological state is accompanied by an appropriate change in the mental emotional
state, conscious or unconscious, and conversely, every change in the mental emotional state, conscious or
unconscious, is accompanied by an appropriate change in the physiological state.
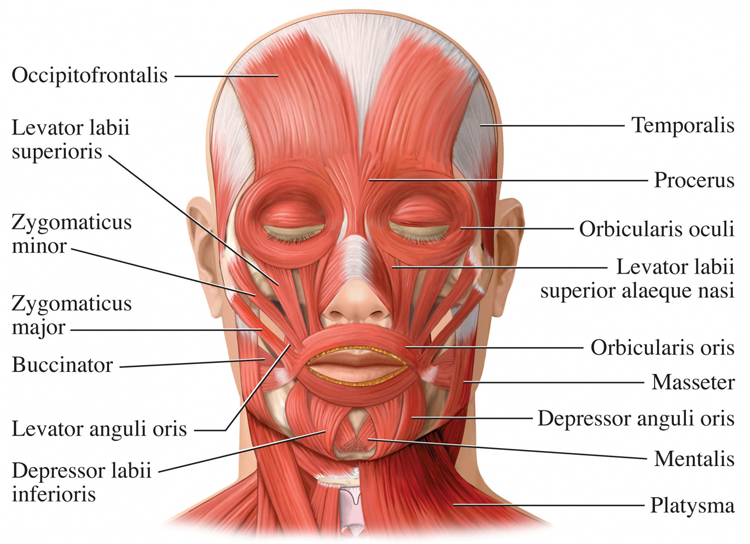
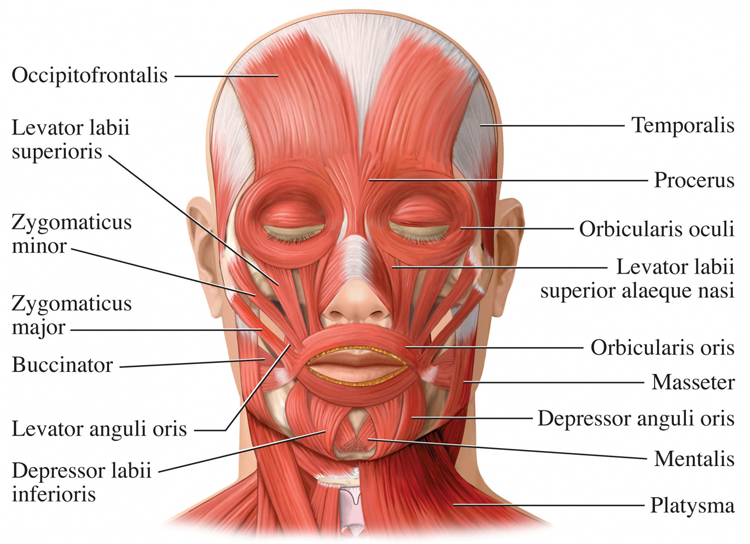
An example of the psychophysiological principle is that facial muscle contraction can influence emotion, and
emotion can influence facial muscle contraction. Botox injections, which paralyze facial muscles to treat
wrinkles, reduce the intensity of a person's emotional experiences. Elmer Green is pictured below.
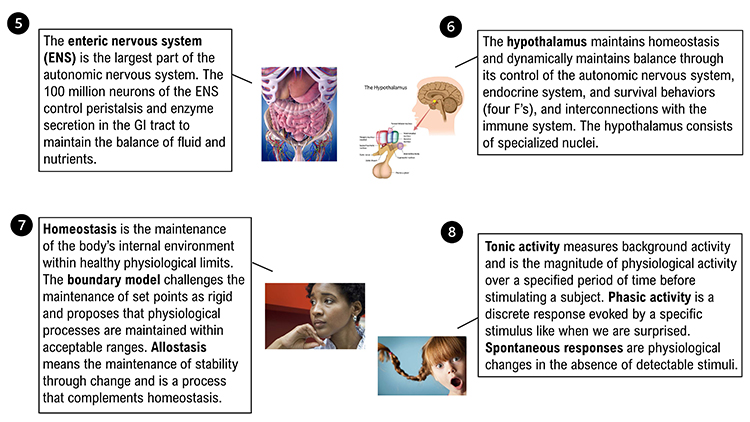
Homeostasis
Homeostasis maintains the body’s internal environment within
healthy physiological limits. Claude Bernard introduced the basic concept
of homeostasis and stated, "The stability of the internal environment is
the condition of a healthy life." Cannon (1939) introduced the term
homeostasis
in 1932 and elaborated on this
concept in
The Wisdom of the Body.

Listen to a mini-lecture on Homeostasis and Allostasis © BioSource Software LLC.
The body achieves homeostasis for
specific variables, like blood pressure, through interlocking negative
and positive feedback systems. Check out the Bozeman Science YouTube video
Positive and Negative Feedback Loops.
Two important modifications to the principle of homeostasis are the boundary model and allostasis.
The
boundary model challenges the maintenance of set points as rigid and proposes
that physiological processes are maintained within acceptable ranges.
Allostasis means the maintenance of stability through change and is a process that
complements homeostasis. Allostasis is achieved by anticipating challenges and adapting through behavior (including learning) and physiological change. Therapists utilize allostasis when they teach patients to use an
abbreviated relaxation exercise (low-and-slow breathing) when they anticipate stressors (traffic jams).
McEwen and Seeman's (1999)
allostatic load model proposes that acute
and repeated stressors can produce harmful physiological changes. Graphic © GalinaPhoto/iStockphoto.com.

Autonomic Balance
Wenger (1972) called the ratio of sympathetic to parasympathetic
activation
autonomic balance. He proposed that resting individuals are
located along a continuum ranging from SNS to PNS dominance.
Normally distributed A-bar scores, which measure location on
this continuum, are calculated from a battery of autonomic measurements.
Low A-bar scores indicate SNS dominance, while high A-bar scores
suggest PNS dominance. Most subjects show intermediate
scores. Wenger and colleagues reported that individuals with low A-bar
scores, whom he called
sympathicotonics, suffered an elevated incidence
of neurotic, psychotic, psychosomatic, and medical disorders.
Generally, low and high A-bar scores seem to predispose individuals to develop psychological and medical disorders. Where
SNS dominance (low
A-bar scores) may result in cardiac arrhythmia and essential
hypertension,
PNS dominance (high A-bar scores) may be
associated with asthma, colitis, and hypotension. Graphic © alexsl/iStockphoto.com.
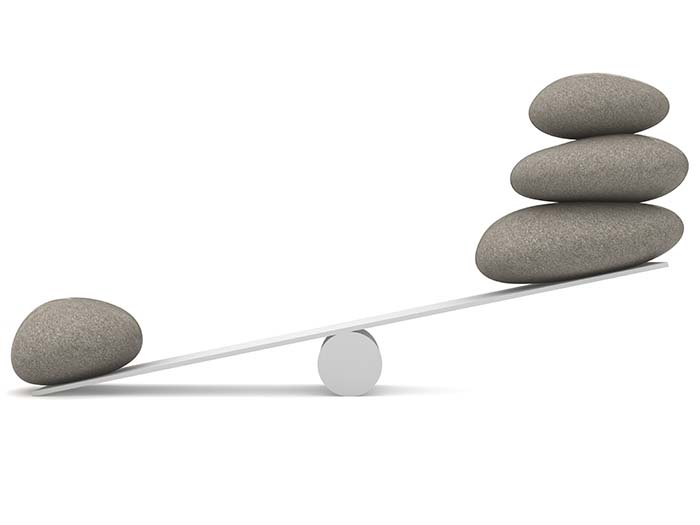
The healthiest pattern
of autonomic balance involves intermediate A-bar scores where neither the
SNS nor the PNS overwhelms the other.
Psychophysiological Measurements
Psychophysiologists monitor tonic, phasic, and spontaneous
psychophysiological activity.
 Listen to a mini-lecture on Tonic and Phasic Activity
Listen to a mini-lecture on Tonic and Phasic Activity © BioSource Software LLC.
Tonic activity measures background activity and is the magnitude of
physiological activity over a specified period before stimulating
the subject. A
resting baseline, where a participant sits quietly without breathing or relaxation instructions, or feedback for 3 or 5 minutes, measures tonic activity. Clinicians obtain pre- and post-baselines to measure the psychophysiological change in variables like heart rate variability or hand temperature within and across training sessions.
Phasic activity is a discrete response evoked by a specific stimulus, like being surprised. Since subjects continuously react to environmental and internal stimuli that we cannot
directly observe, interpreting phasic activity can be challenging. Graphic © ideabug/iStockphoto.com.

Spontaneous responses are physiological changes in the absence of
detectable stimuli. These changes are important to researchers because
they can confound the measurement of phasic activity. For example, suppose a spontaneous increase in skin conductance occurs as a subject is shown an emotionally-charged slide. In that case, a researcher could mistakenly conclude that the slide increased conductance more than it did (Stern, Ray, & Quigley,
2001).
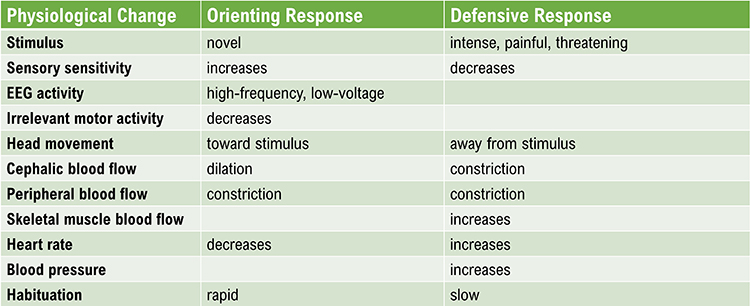
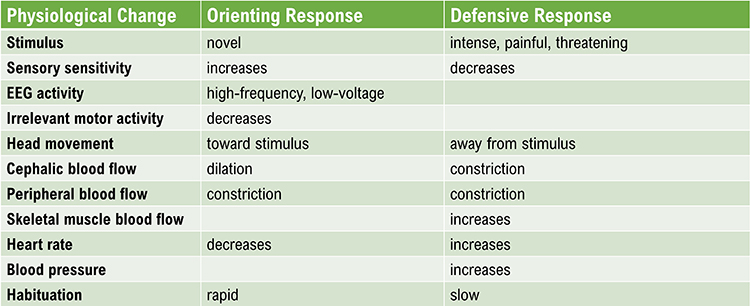
Orienting and Defensive Responses
When exposed to a novel stimulus, an orienting response prepares us to deal with this challenge.
Pavlov's (1927)
orienting response is a "What
is it?" reaction to stimuli like the sound of a vase crashing. The orienting response includes (1) increased
sensory sensitivity, (2) head (and ear) turning toward the stimulus, (3) increased muscle tone (reduced movement),
(4) EEG desynchrony, (5) peripheral constriction and cephalic vasodilation, (6) a rise in skin conductance, (7)
heart rate slowing, and (8) slower, deeper breathing. An orienting response rapidly habituates since it is no
longer needed once we respond to a novel stimulus.
In contrast, a
defensive response is a slowly habituating response
pattern that limits harm from intense stimulation. This pattern includes (1) reduced sensory sensitivity, (2) a
tendency to move away from the stimulus, (3) heart rate increase, and (4) both peripheral and cephalic
vasoconstriction. For example, a loud noise in a workplace environment might elicit a defensive response.
Activation and Habituation
Activation was Duffy’s (1972) term for arousal.
Activation
This concept originated
in Cannon's (1915) idea of the body's integrated preparation to fight or
flee a potential threat. Activation implies a unidimensional continuum
that ranges from low to high activation. For example, high activation
might be associated with elevated blood pressure, heart rate, and
respiration rate. Low activation might be associated with reduced
responses to these variables.
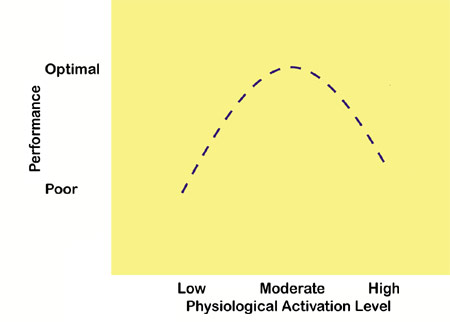
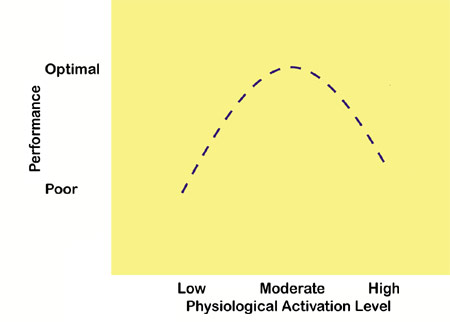
Duffy (1957) hypothesized that performance rises with increased
physiological arousal to an optimal level for a specific task
and then declines with further arousal. This relationship is an
inverted
U-shaped curve. Task complexity and novelty may determine the optimal
level of arousal. The optimal level of arousal will be lower for more
complex and novel tasks. John Balven created the illustration below.
Problems with Activation Theory
Lacey (1967) and others have strongly criticized activation theory. The main
concerns are that arousal is not a single dimension. Individuals show unique response patterns, different stimuli
elicit specific response patterns in most people, other emotions are associated with distinct physiological
changes, and responses can be complex.
1. Lacey argued that
arousal is not a single dimension. He believed that researchers should
differentiate between autonomic, behavioral, and cortical arousal since these different forms of arousal are not
interchangeable. For example, when heterosexual men observe slides of nude women, heart rate may increase while
finger blood flow may not change. If we only use finger blood flow as our index of arousal, we might mistakenly
conclude that the male subjects are not aroused (Stern, Ray, & Davis, 1980).
2. Individuals exhibit unique response patterns, called a
response
stereotypy, in which they show consistent physiological responses when encountering stimuli that
share the same intensity and elicit similar emotions. For example, a patient may raise her heart rate and blood
pressure when delivering a report during a business meeting or completing an assignment under time pressure.
Individual response stereotypy occurs because our clients possess different diatheses (vulnerabilities) and
enter treatment with unique learning histories. During an assessment, a clinician conducts a psychophysiological
profile (PSP) to determine a client's response stereotypy by presenting several mild stressors.
3. Specific stimuli elicit a distinctive response pattern in most participants instead of simply altering
activation. This is the principle of
stimulus-response specificity. For
example, individuals may increase their skeletal muscle tone when challenged to compete.
Situational specificity is an example of stimulus-response specificity. It means that a physiological response
(blood pressure elevation) does not occur randomly and is most likely in situations with unique
characteristics. A situation's properties may include the location (office), time of day (morning),
activity (conference), individuals present (employer), and personal emotional state (anxiety).
A client's elevated blood pressure may be classically or operantly conditioned. They may be
unaware of learning this response since its symptoms are largely "silent" and both processes involve
implicit learning. Due to associative learning, the presence of one or more situational cues may elicit a complete physiological response.
Clinicians investigate the situational specificity of presenting complaints when they conduct a history,
perform a psychophysiological profile (PSP), ask the client to maintain a symptom journal, and monitor the
client in multiple real-world settings (blood pressure measurement in the office and while stalled in traffic).
Situational information is crucial to creating stimulus hierarchies when using systematic desensitization
to treat a phobia.
4. Primary emotions are associated with unique physiological changes. This is the concept of
emotional response specificity. The six primary facial expressions are surprise,
anger, sadness, disgust, fear, and happiness.
Research by Ekman and colleagues with facial expressions showed that anger increases heart rate and skin
temperature, fear increases heart rate, and decreases skin temperature. Happiness increases heart rate but
does not affect skin temperature.
Schwartz, Weinberger, and Singer (1981) studied cardiovascular patterning
in six emotions using imagery, nonverbal expression, and exercise tasks. Their dependent variables were
diastolic and systolic blood pressure and heart rate. Participants' cardiovascular responses distinguished
anger from fear (blood pressure) and anger and fear from happiness and sadness.
Ax (1953) reported that 7 of 14 autonomic measures discriminated between
fear and anger.
5. Responses to a stimulus can be complex, with some physiological indices increasing and others decreasing.
This builds on the principle of stimulus-response specificity. Specific stimuli elicit a distinctive response
pattern, which is often complex. Lacey called this intricate pattern
directional
fractionation. For example, when a Capitol Hill police officer hears a noise, EEG and
skin conductance may increase cortical activation while GI tract activity decreases.
Habituation
Habituation is the opposite of arousal. A person gradually ceases to
respond or reduces their response to a constant stimulus.
For
example, after 15 trials of listening to a moderate intensity tone, heart
rate might no longer increase. Predictable, low-intensity stimuli that
convey no new information and require no response readily produce
habituation. Habituation is inhibited when a stimulus is intense,
complex, and unique, and the subject must respond to it (rate its
unpleasantness).
The orienting response and defensive response differ in their speed of
habituation. Orienting responses rapidly habituate, while defensive
responses habituate very slowly.
Situational Specificity
Situational specificity means that a
physiological response (blood pressure elevation) does not occur randomly
and is most likely in situations with special characteristics.
A
situation's properties may include the location (office), time of
day (morning), activity (conference), individuals present (employer), and
personal emotional state (anxiety). A client's hypertensive response may
be classically or operantly conditioned, which means they may
be unaware of learning this response since its symptoms are largely
"silent," and both processes involve implicit learning. Due to associative
learning, the presence of one or more situational cues may elicit a
complete physiological response.
Clinicians investigate the situational specificity of presenting
complaints when they conduct a history, perform a psychophysiological
profile (PSP), ask the client to maintain a symptom journal, and monitor
the client in multiple real-world settings (blood pressure measurement in
the office and while stalled in traffic). Situational information is
crucial in creating stimulus hierarchies when using systematic
desensitization to treat a phobia.
Law of Initial Values (LIV)
Wilder (1967) argued that the size of our response to a stimulus depends
on a physiological variable's starting value.
Wilder’s
law of initial
values (LIV) predicts that the higher the initial value of a
physiological variable, the less its tendency to change. For example, a
subject who normally breathes rapidly should only slightly increase their respiration rate when exposed to a loud sound. Homeostatic
mechanisms (negative feedback) are responsible for this phenomenon.
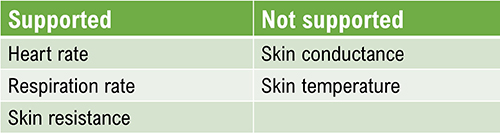
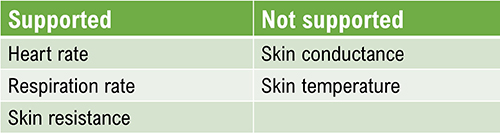
Hord, Johnson, and Lubin (1964) found that the LIV applies to heart and respiration rates but not to skin conductance or skin temperature.
Stern, Ray, and Quigley (2001) reported that studies support the LIV for
heart rate and skin resistance but not for skin conductance.
Berntson and colleagues (1994) questioned the LIV's value and encouraged researchers to develop an "autonomic constraints" model tied to underpinning physiology.
Relevance of the LIV for Biofeedback
Researchers studying
phasic (rapidly changing) measures may consider
employing statistical methods to control the influence of prestimulus
values on the size of physiological responses.
The LIV is a
principle—not a
law—and does
not apply to all subjects and
response systems. Jamieson (1993)
questioned the LIV’s value for psychophysiological research since it can
be influenced by several factors (measurement errors, reactivity or
response to the measurement process, skew or asymmetrical distribution
of scores, and variance or difference among scores).
Researchers can determine whether the LIV is relevant by
computing the
correlation between prestimulus and poststimulus values.
Geenen and van
de Vijver (1993) suggested that the LIV may be less common than perceived
and correction methods may harm the data more than the
phenomenon itself.
Generalization of Biofeedback Training
The key muscle hypothesis and hand-warming specificity have
important implications for biofeedback training.
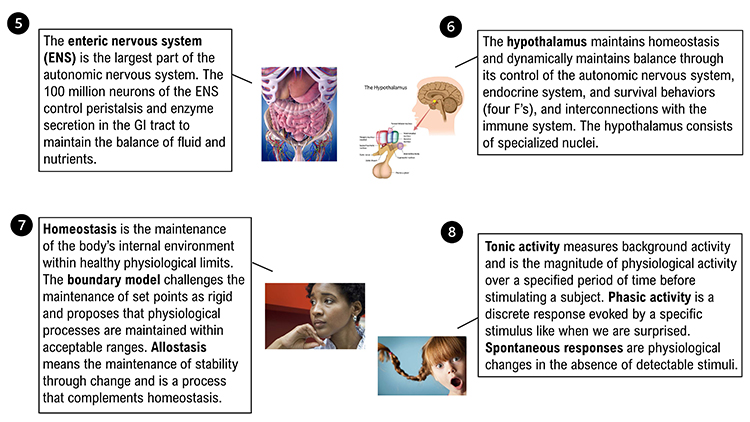
Key Muscle Hypothesis
The
key muscle hypothesis is the proposition that a single muscle indexes
activity in other muscle groups. Research strongly contradicts this view:
(1) SEMG values across different sites are uncorrelated, (2) single-site
SEMG values are not correlated with generalized tension or autonomic
arousal, and (3) SEMG reductions at one site (frontalis) do not
automatically generalize to other sites.
The key muscle hypothesis is invalid because there is no key upper body
or lower body muscle group. The musculoskeletal system functions very
specifically--we simultaneously contract and relax adjacent
agonist-antagonist muscle pairs at a joint. This belief has resulted in
clinicians mistakenly training the
frontalis muscle to lower autonomic
arousal or relax muscles on the upper trunk.
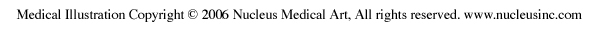
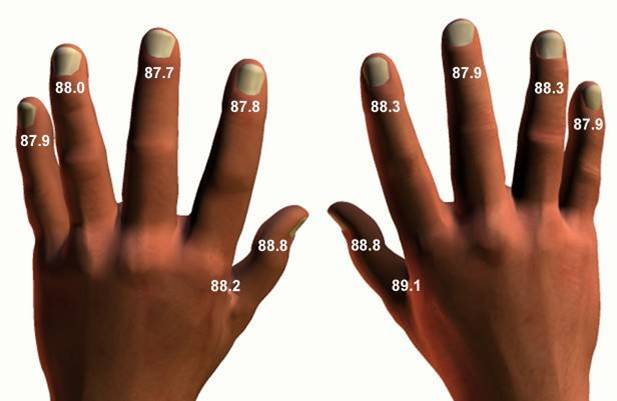
Hand-Warming Specificity
The cardiovascular system can function very precisely, just like the
musculoskeletal system. Temperature training can produce extremely
site-specific changes. For example, vasodilation in the right hand need
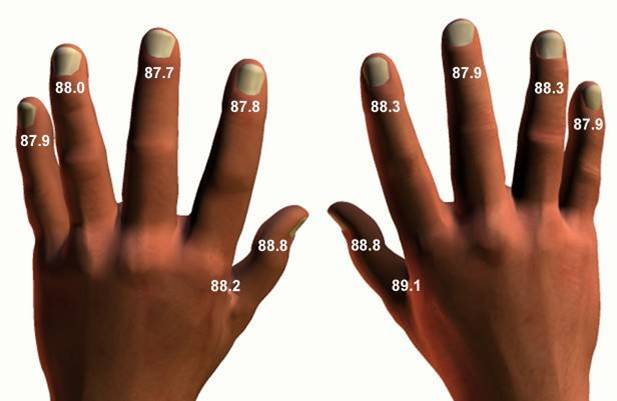
not generalize to the left hand or the feet. The picture below shows the placement of a
thermistor (temperature sensor) on the index finger's dorsal surface.

Clinicians should never expect hand-warming to generalize beyond the
actual site (digit) trained. Depending on training procedure and
individual differences, hand-warming might generalize to other digits on
the same hand or to the other hand for some clients but
not for others.
The temperature map below shows mean undergraduate finger and web dorsum temperatures
(Lammy et al., 2004).
The Placebo Effect
Placebos are inert interventions that can
produce a significant clinical response. Both the symptoms and therapeutic response are real and measurable in a placebo response.
 Listen to a mini-lecture on the Placebo Effect
Listen to a mini-lecture on the Placebo Effect © BioSource Software LLC. Check out Eric Mead's TED Talk The
Magic of the Placebo. Graphic © kasezo/Shutterstock.com.

Placebos can be pharmacological (e.g., drug), procedural (e.g., osteopathic manipulation), psychological (e.g.,
conversation), and environmental (e.g., the clinic setting).
Contrary to clinical lore:
(1) The percentage of patients who improve with a placebo can exceed 60%.
(2) Placebo responses can last as long as improvement with prescription drugs.
(3) Placebos are more effective when closely following effective medication (classical conditioning and
expectancy).
(4) Effective medication is less effective when it follows ineffective medication (classical conditioning and
expectancy).
(5)
Open-label placebos, where patients are told they receive placebos, can produce clinical improvement (Schaefer et al., 2018).
An
active placebo, which adds an ingredient that produces an unrelated side
effect, yields a therapeutic response in about 60% of people. Prescription drugs elicit a therapeutic
response in 50% (actual practice) to 70% (supervised drug trial) of the population.
Placebos have the most significant effects on symptoms or disorders that wax and wane over time (e.g., major
depression and chronic pain). The placebo response to drug treatment of depression increases by about 7% per
decade (Advokat, Comaty, & Julien, 2019).
Placebos seem to trigger a homeostatic response via stimulus-response
learning, expectancy, and the release of endogenous neurotransmitters
like endorphins and adrenaline-like catecholamines. This may mirror
changes (therapeutic effects, time course, and duration of effect)
produced by prescription drugs.
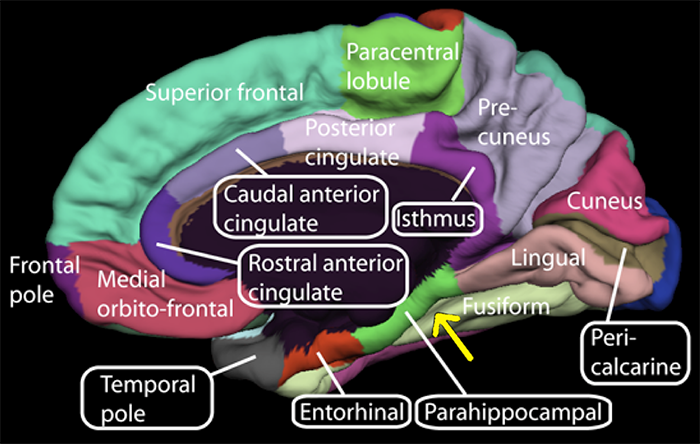
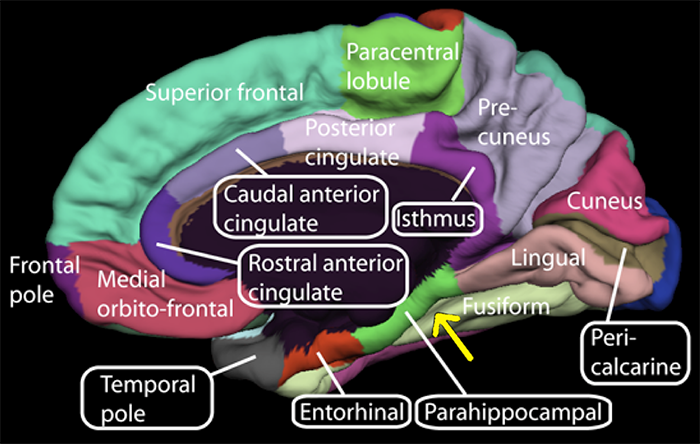
Petrovic and colleagues (2002) showed
that opioid analgesia and placebo analgesia increased
activity in the rostral anterior cingulate cortex and the brainstem.
Wager et al.
(2004) used the
functional MRI (fMRI) to
study the placebo effect. They exposed volunteers to painful shocks or
heat. Participants told that an "anti-pain cream" had been applied to their arms
reported less pain than those not told about the cream. The
fMRI showed that participants in the "anti-pain" cream condition increased
activity in the prefrontal cortex and decreased activity in
pain-processing regions of the thalamus, somatosensory cortex, and
cerebral cortex.
Kaptchuk et al. (2010) reported the results of a randomized controlled study
of 80
Irritable Bowel Syndrome (IBS) patients. Fifty-nine percent of those
told that they would receive inert pills and that ‘‘placebo pills, something like sugar
pills, have been shown in rigorous clinical testing to produce significant mind-body self-healing processes’’
improved. In contrast, only 35% of patients randomly assigned to a no-treatment control group showed gains.
Right parahippocampal gyrus (r-PHG) connectivity measured using fMRI scans predicted placebo-mediated analgesia in patients diagnosed with chronic knee osteoarthritis (Tétreault et al., 2016). Graphic courtesy of Wikimedia Commons.
Inter-Brain Synchrony
Therapy provides a structured environment where patients can repeatedly experience and strengthen inter-brain synchrony (Meehan, 2025; Sened et al., 2022). In
inter-brain synchrony, the neural activity of two individuals becomes aligned during social interactions. This synchrony is observed in therapeutic settings when a therapist and a patient engage in shared emotional and cognitive processes, such as maintaining eye contact, mirroring expressions, and synchronizing speech rhythms. This mutual alignment of brain activity, often termed neural coupling, facilitates a deeper interpersonal connection and effective communication Over time, this repeated neural coupling can lead to lasting neurobiological adaptations, reinforcing healthier emotional and cognitive frameworks. Vagus nerve graphic © Axel_Kock/Shutterstock.com.

Further evidence suggests that synchrony strengthens emotional bonds and improves cognitive flexibility. When neural coupling occurs, it facilitates better communication between brain regions associated with decision-making, problem-solving, and emotional processing. This may explain why clients who engage in therapy with high levels of synchrony often experience deeper insights, improved emotional resilience, and greater capacity for behavioral change. Understanding and intentionally fostering this synchrony can, therefore, be a powerful tool in therapeutic practice, enhancing the overall efficacy of interventions.
For therapists, these findings underscore the importance of fostering therapeutic synchrony as an active component of treatment. Beyond verbal communication, nonverbal cues such as body language, tone of voice, and paced responsiveness contribute significantly to inter-brain synchrony. Therapists who practice mindfulness, attunement, and embodied presence may enhance their ability to facilitate neural synchrony with clients, potentially amplifying the effectiveness of therapy.
Moreover, this perspective encourages therapists to view relational healing not only as a psychological process but also as a neurobiological one. Clients who struggle with attachment issues, social difficulties, or trauma may particularly benefit from interventions that emphasize relational presence, attunement, and co-regulation.
Relational presence refers to the therapist’s capacity to fully engage with the client, establishing an environment of genuine connection and trust where the client feels seen and valued.
Attunement is the process by which the therapist accurately perceives and sensitively responds to the client’s emotional signals, thereby fostering a therapeutic interaction that validates the client’s internal experience.
Co-regulation involves a collaborative dynamic in which the therapist supports the client in managing and modulating their emotional states, ultimately aiding the client in developing effective self-regulation skills. Collectively, these processes help create a secure relational framework essential for healing and developing adaptive emotional responses.
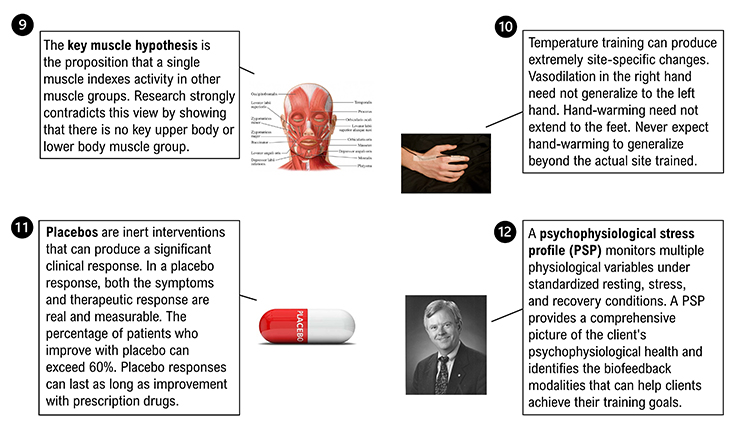
Psychophysiological Assessment
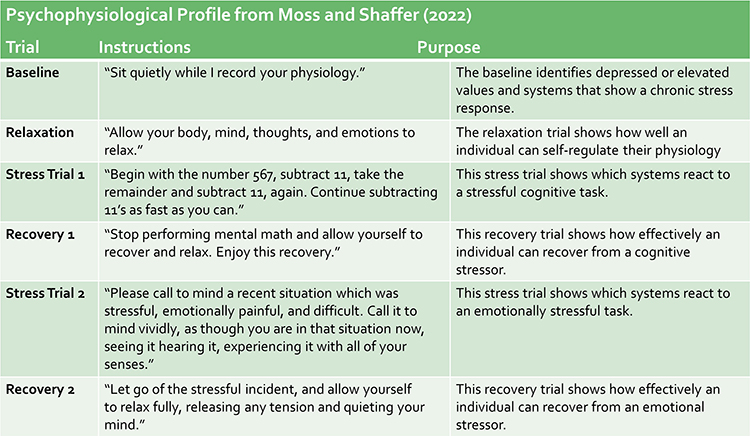
Client assessment is a collaborative process that starts with an orientation to biofeedback, client recording symptoms, a psychophysiological history, referral to physicians to investigate related medical complaints, and a psychophysiological stress profile (Moss & Shaffer, 2022).

Caption: Don Moss
Psychophysiological Stress Profile Overview
A
psychophysiological stress profile (PSP) monitors multiple physiological variables under standardized resting, stress, and recovery conditions. Clinicians use a PSP to detect chronic problems that depress or elevate physiological measures, overactivation in response to stressors, and difficulty recovering from stress trials. A PSP provides a comprehensive picture of the client's psychophysiological health and identifies the biofeedback modalities to help clients achieve their training goals.
In a typical PSP, a practitioner will monitor hand temperature (TEMP), heart rate (HR) and heart rate variability (HRV), respiration (RESP), skeletal muscle electrical activity (SEMG), skin conductance (SCL), and possibly brain electrical activity (EEG). The clients' presenting complaints may determine the placement of SEMG and EEG sensors. For example, a clinician may use left and right SEMG channels to record cervical paraspinal muscle activity in tension-type headaches.
PSP Structure
A clinician may divide the PSP into a 5-minute baseline (no feedback or breathing instructions), a 3-minute relaxation period (relaxation instructions), a 3-minute stress trial (e.g., visualizing a recent stressful event), a 3-minute recovery period, a second 3-minute stress trial, and a final 3-minute recovery period.
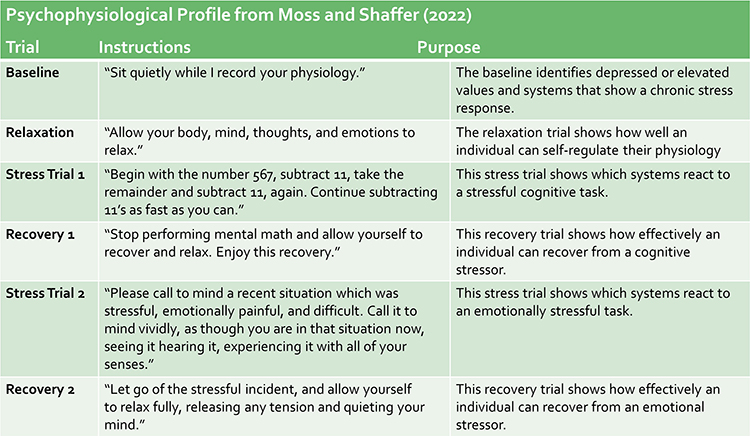
How the PSP Can Guide Treatment Planning
The PSP
provides extensive information about a client's psychophysiology to guide treatment planning. Instead of a manualized "one size fits all" approach, the PSP enables a practitioner to tailor training to a client's unique strengths and needs.
First, the baseline reveals which values are depressed or elevated. This can help identify systems that are dysregulated in everyday life. Second, the relaxation trial evaluates a client's ability to self-regulate their physiology. Third, the stress trials show which systems over or under react to cognitive and emotional challenges. Fourth, the recovery trials assess a client's ability to restore relaxed physiology following stressors.
When the Psychophysiological History and PSP identify a distinct stereotypy, a practitioner can target the systems that may contribute to a client's systems. For example, a practitioner might recommend muscle relaxation training if a client's upper back and neck muscles were excessively tense during baseline, did not loosen during relaxation, tensed further during both stressors, and did not recover following the stressors.

Glossary
A-bar: Wenger’s shorthand for the ratio of sympathetic to
parasympathetic excitation. Patients with low A-bar scores are sympathetic-dominant, and those with high A-bar
scores are parasympathetic dominant.
accentuated antagonism:
the parasympathetic nervous system's ability to directly oppose sympathetic action, such as slowing the heart by 20 or 30 beats.
activation: Duffy’s term for arousal originated with Cannon’s fight-or-flight
response.
active placebo: a placebo combined with an additive to produce a side effect
that can elicit a therapeutic response rate in about 60% of patients.
allostasis: the maintenance of stability through change by mechanisms that
anticipate challenges and adapt through behavioral and physiological change.
allostatic load model: McEwen and Seeman’s hypothesis that biological responses to stress can harm the body when stressors are acute or repeatedly occur.
attunement: the process by which a therapist accurately perceives and responds to a clients emotional state.
autonomic balance: Wenger’s concept of a ratio of sympathetic to
parasympathetic excitation.
autonomic nervous system: the subdivision of the peripheral nervous system that includes enteric, parasympathetic, and sympathetic.
boundary model: the position that setpoints are not rigid and that physiological
processes are maintained within acceptable ranges.
central nervous system: the division of the nervous system that includes the
brain, spinal cord, and retina.
co-regulation: the process through which one person helps another regulate their emotional state through interaction and connection.
defensive response: a very slowly habituating response pattern that limits
harm from intense stimulation. This pattern includes (1) reduced sensory sensitivity, (2) a tendency to move away
from the stimulus, (3) heart rate increase, and (4) both peripheral and cephalic vasoconstriction.
diathesis: vulnerability. For example, a genetic predisposition to gain
weight.
directional fractionation: Lacey’s concept of a complex pattern of
physiological response to a stimulus where some indices increase and others decrease.
emotional response specificity: the hypothesis that primary emotions are
associated with unique physiological changes.
enteric division: a subdivision of the autonomic nervous system that regulates
the gut and is innervated by sympathetic and parasympathetic branches.
epinephrine: an adrenal medullary hormone that increases muscle blood flow, converts stored nutrients into glucose for use by skeletal muscles, and initiates cardiac muscle contraction when it binds to ß1 receptors.
freeze response: immobilization when facing a threat you cannot fight or flee.
functional MRI (fMRI): magnetic resonance imaging procedure that can detect
small changes in brain metabolism.
habituation: the weakening or disappearance of a response to a constant
stimulus.
heart rate variability (HRV): the organized fluctuation of time intervals between successive heartbeats defined as interbeat intervals.
homeostasis: the state of dynamic constancy achieved by stabilizing conditions
about a setpoint, whose value may change over time.
homeostat: device that maintains homeostasis. For example, the hypothalamus.
hypothalamus: the forebrain structure below the thalamus that dynamically
maintains homeostasis controlling the autonomic nervous system, endocrine system, survival behaviors,
and interconnections with the immune system.
idiographic approach: a research strategy that emphasizes individual
differences.
inter-brain plasticity: the capacity of the brain to adapt and change based on repeated neural synchrony with another person.
key muscle hypothesis: the discredited proposition that a single muscle indexes
activity in other muscle groups.
law of initial values: Wilder’s proposition that the size of our
response to a stimulus depends on a physiological variable's starting value. This principle has only been
demonstrated for heart rate, respiration rate, and skin resistance.
mass activation: the simultaneous stimulation of adjacent ganglia (cell bodies) in
the sympathetic chain during emergencies allows the sympathetic nervous system to produce many coordinated changes at once. For
example, increased heart rate, respiration rate, and sweat gland activity.
medulla: a brainstem structure that regulates blood pressure, defecation, heart
rate, respiration, vomiting, the autonomic nervous system, and distributes signals between the brain and spinal
cord.
neural coupling: the synchronization of brain activity between two individuals during social or therapeutic interactions.
norepinephrine: an adrenal medullary hormone that increases muscle blood flow and
converts stored nutrients into glucose for skeletal muscles.
open-label placebo: an inert treatment disclosed as a placebo to patients.
orienting response: Pavlov’s "What is it?" reaction to stimuli
like the sound of a vase crashing that includes (1) increased sensory sensitivity, (2) head (and ear) turning
toward the stimulus, (3) increased muscle tone (reduced movement), (4) EEG desynchrony, (5) peripheral
constriction and cephalic vasodilation, (6) a rise in skin conductance, (7) heart rate slowing, and (8) slower,
deeper breathing.
parasympathetic division: the autonomic nervous system subdivision that regulates
activities that increase the body’s energy reserves, including salivation, gastric (stomach) and intestinal
motility, gastric juice secretion, and increased blood flow to the gastrointestinal system.
parasympathetic dominance: Wenger’s concept of greater parasympathetic
activation than sympathetic activation.
peripheral nervous system: nervous system subdivision that includes autonomic
and somatic branches.
phasic: a brief change in physiological activity in response to a discrete
stimulus. For example, a single skin potential response in reaction to a sudden tone.
placebo: an inert intervention that can produce a therapeutic response rate in
about 30% of patients.
polyvagal theory: the theory that the unmyelinated vagus (dorsal vagus complex) and newer myelinated vagus (ventral vagal complex) mediate competing adaptive responses.
psychophysiological principle: Green, Green, and Walter’s concept that
there is a bidirectional relationship between physiological and psychological functioning. For example, facial
muscle contraction can influence emotion, and emotion can influence facial muscle contraction.
Psychophysiological Stress Profile (PSP): structured assessment procedure that monitors multiple physiological variables under standardized resting, stress, and recovery conditions.
relational presence: a therapist's ability to be fully engaged and attuned to a client in a way that fosters connection and trust.
response stereotypy: a consistent pattern of physiological responses when an
individual encounters stimuli with the same intensity and elicit similar emotions. For example, a patient
may raise her heart rate and blood pressure when delivering a report during a business meeting or completing an
assignment under time pressure.
resting baseline: a tonic measure of psychophysiological activity (e.g., temperature) without breathing or relaxation instructions and feedback.
situational specificity: the occurrence of a physiological response in
specific situations. For example, blood pressure increase during a dental examination.
somatic nervous system: the peripheral nervous system subdivision that receives
external sensory and somatosensory information and controls skeletal muscle contraction.
spontaneous responses: physiological changes in the absence of detectable
stimuli. For example, skin conductance responses when no tones are presented to a subject.
stimulus-response specificity: specific stimuli elicit a distinctive response
pattern in most individuals instead of simply altering activation. For example, subjects may increase their skeletal
muscle tone when challenged to compete.
sympathetic dominance: Wenger’s concept of greater sympathetic
activation than parasympathetic activation.
sympathetic nervous system: the autonomic nervous system branch that regulates
activities that expend stored energy, such as when we are excited.
sympathicotonics: Wenger’s term for sympathetic-dominant individuals
who they hypothesized to suffer an elevated incidence of neurotic, psychotic, psychosomatic, and medical
disorders.
therapeutic synchrony: the alignment of emotional and cognitive processes between therapist and client that enhances the therapeutic process.
tonic: a background level of physiological activity. For example, a 5-minute
average of hand temperature.
vagal withdrawal: the inhibition of the myelinated vagus, often by daily stressors.
Test Yourself
Click on the ClassMarker logo to take 10-question tests over this unit without an exam password.

REVIEW FLASHCARDS ON QUIZLET
Click on the Quizlet logo to review our chapter flashcards.

Visit the BioSource Software Website
BCIA offers two HRV Biofeedback Certification paths: Biofeedback and Neurofeedback.
For Biofeedback, BioSource Software offers
Human Physiology to satisfy BCIA's Human Anatomy & Physiology requirement. For Neurofeedback, BioSource provides
Physiological Psychology to satisfy BCIA's Physiological Psychology requirement.
BCIA has accredited each course, and they combine affordable pricing ($150) with industry-leading content.

Essential Skills
1. Interview a client about the history and prior treatment of the presenting complaints, the individual’s
life situation, including stressors and resources, and her understanding of the cause(s) and consequences of these
symptoms.
2.
Explain the purpose and procedures of a psychophysiological profile to a client.
3. Administer a psychophysiological profile to a client utilizing several modalities and containing pre-baseline, stressor, recovery, and relaxation conditions. Explain your selection of the modalities and placements used.
4. Demonstrate how to detect and remove artifacts from the raw signals that were monitored.
5. Evaluate and summarize the findings of the psychophysiological profile, relate them to the client’s
presenting complaints, and identify training goals based on these data.
6. Explain the results from the psychophysiological profile and training goals to your client.
7. Develop a treatment plan for your client based on the interview and psychophysiological profile.
8. Explain the treatment plan to your client.
Assignment
Now that you have completed this unit, how might it change how you explain psychophysiological concepts like
the autonomic nervous system to your clients?
References
Advokat, C. D., Comaty, J. E., & Julien, R. M. (2019).
Julien's primer of drug action (14th ed.). Worth Publishers.
Andreassi, J. L. (2007).
Psychophysiology: Human behavior and
physiological response (5th ed.)
. Lawrence Erlbaum Associates,
Publishers.
Begley, S. (2005). How mirror neurons help us empathize, really feel
others' pain.
The Wall Street Journal, B1.
Berntson, G. G., Cacioppo, J. T., & Quigley, K. S. (1993).
Cardiac psychophysiology and autonomic space in humans: Empirical perspectives and conceptual implications.
Psychological Bulletin, 114, 296-322. https://doi.org/10.1037/0033-2909.114.2.296
Berntson, G. G., Urchino, B. N., & Cacioppo, J. T. (1994). Origins of baseline variance and the Law of Initial Values.
Psychophysiology, 31(2), 204-210. https://doi.org/10.1111/j.1469-8986.1994.tb01042.x
Brannon, L., Updegraff, J. A., & Feist, J. (2022).
Health psychology: An introduction to behavior and health (10th ed.). Wadsworth.
Breedlove, S. M., & Watson, N. V. (2020).
Behavioral neuroscience (9th ed.)
. Sinauer Associates, Inc.
Cacioppo, J. T., Tassinary, L. G., & Berntson, G. G. (Eds.). (2007).
Handbook of
psychophysiology (3rd) ed.)
. Cambridge University Press.
Coull, J. A., Beggs, S., Boudreau, D., Boivin, D., Tsuda, M., Inoue, K., Gravel, C., Salter, M. W., & De Konink, Y. (2005).
BDNF from microglia causes the shift in neuronal anion gradient underlying neuropathic pain.
Nature, 438,
1017-1021. https://doi.org/10.1038/nature04223
Dahr, A. K., Lambert, G. W., & Barton, D. A. (2016). Depression and cardiovascular disease: Psychopbiological mechanisms.
In M. E. Alvarenga, & D. Byrne (Eds.).
Handbook of psychocardiology. Springer Singapore.
Fox, S. I., & Rompolski, K. (2022).
Human physiology (16th ed.). McGraw-Hill.
Gevirtz, R. (2013). The nerve of that disease: The vagus nerve and cardiac rehabilitation.
Biofeedback, 41, 32-38. https://doi.org/10.5298/1081-5937-41.1.01
Green, E., Green, A. M., & Walters, E. D. (1970). Voluntary control of internal states: Psychological and physiological.
Journal of Transpersonal Psychology, 2, 1-26.
Gurung, R. A. R. (2018).
Health psychology: Well-being in a diverse world (4th ed.). Thompson
Wadsworth.
Hugdahl, K. (1995).
Psychophysiology: The mind-body perspective. Harvard University
Press.
Kaptchuk, T. J., Friedlander, E., Kelley, J. M., Sanchez, M. N., Kokkotou, E., Singer, J. P., Kowalczykowski, M., Miller, F. G., Kirsch, I., & Lembo, A. J.
(2010).
Placebos without deception: A randomized controlled trial in Irritable Bowel Syndrome.
PLoS ONE 5(12),
e15591. https://doi.org/10.1371/journal.pone.0015591.
Khazan, I. Z. (2013).
The clinical handbook of biofeedback: A step-by-step guide for training and practice with mindfulness. John Wiley & Sons, Ltd.
Khazan (2019). A guide to normal values for biofeedback. In D. Moss & F. Shaffer (Eds.).
Physiological recording technology and applications in biofeedback and neurofeedback
(pp. 2-6). Association for Applied Psychophysiology and Biofeedback.
Kingsley, R. E. (2000).
Concise textbook of neuroscience (2nd
ed.). Lippincott Williams & Wilkins.
LeDoux, J. (2002).
Synaptic self. Viking Penguin.
Malta, L. S., Blanchard, E. B., Freidenberg, B. M., Galovski, T. E.,
Karl, A., & Holzapfel, S. R. (2001).
Psychophysiological reactivity of aggressive drivers: An exploratory study.
Applied Psychophysiology and
Biofeedback, 26(2), 95-116.
Meehan, Z. M. (2025). 5-min science: Inter-brain plasticity can enhance psychotherapy. https://www.biosourcesoftware.com/post/5-min-science-inter-brain-plasticity-can-enhance-psychotherapy
Moss, D., & Shaffer, F. (2022).
A
primer of biofeedback. Association for Applied Psychophysiology and Biofeedback.
Nunan, D., Sandercock, G. R. H., & Brodie, D. A. (2010).
A quantitative systematic review of normal values for short-term heart rate variability in healthy adults.
Pacing and Clinical Electrophysiology, 33(11), 1407-1417. https://doi.org/10.1111/j.1540-8159.2010.02841.x
Olshansky, B., Sabbah, H. N., Hauptman, P. J., & Colucci, W. S. (2008).
Parasympathetic nervous system and heart failure: Pathophysiology and potential implications for therapy.
Circulation, 118, 863-871. https://doi.org/10.1161/CIRCULATIONAHA.107.760405
Pennebaker, J. W., Kiecolt-Glaser, J. K., & Glaser, R. (1988).
Disclosure of traumas and immune function: Health implications for psychotherapy.
Journal of Consulting and Clinical Psychology, 56, 239-245. https://doi.org/10.1037//0022-006x.56.2.239
Petrovic, P., Kalso, E., Petersson, K. M., & Ingvar, M. (2002).
Placebo and opioid analgesia--Imaging a shared neuronal network.
Science,
295, 1737-1740. https://doi.org/10.1126/science.1067176
Pinel, P. J., & Barnes, S. (2017).
Biopsychology (10th ed.). Pearson
Education, Inc.
Poole, L., Dickens, C., & Steptoe, A. (2011).
The puzzle of depression and acute coronary syndrome: Reviewing the role of acute inflammation.
Journal of Psychosomatic Research, 71(2), 61-68. https://doi.org/10.1016/j.jpsychores.2010.12.009
Porges, S. W. (2011).
The polyvagal theory: Neurophysiological foundations of emotions, attachment,
communication, and self-regulation. W. W. W. Norton & Company.
Rao, M., & Gershon, M. D. (2016). The bowel and beyond: The enteric nervous system in neurological disorders.
Nature Reviews Gastroenterology & Hepatology, 13, 517–528. https://doi.org/10.1038/nrgastro.2016.107
Rizzollati, G., & Sinigaglia, C. (2006).
Mirrors in the brain. Oxford University Press.
Schwartz, G. E., Weinberger, D. A., & Singer, J. A. (1981).
Cardiovascular differentiation of happiness, sadness, anger, and fear following imagery and exercise.
Psychosomatic Medicine,
43, 343-364. https://doi.org/10.1097/00006842-198108000-00007
M. S.
Schwartz, & F. Andrasik (Eds.). (2003).
Biofeedback: A practitioner's guide
(3rd ed.). The Guilford Press.
Schwartz, S. (2015). Viva vagus: Wandering nerve could lead to range of therapies.
Science News, 188(11), 18.
Schaefer, M., Sahin, T., & Berstecher, B. (2018). Why do open-label placebos work? A randomized controlled trial of an open-label placebo induction with and without extended information about the placebo effect in allergic rhinitis.
Plos One, 13,(3), e0192758. https://doi.org/10.1371/journal.pone.0192758. eCollection 2018
Sened, H., Zilcha-Mano, S., & Shamay-Tsoory, S. (2022). Inter-brain plasticity as a biological mechanism of change in psychotherapy: A review and integrative model.
Frontiers in Human Neuroscience, 16, 955238. https://doi.org/10.3389/fnhum.2022.955238
Shaffer, F., McCraty, R., & Zerr, C. L. (2014).
A healthy heart is not a metronome: An integrative review of the heart’s anatomy and heart rate variability.
Frontiers in Psychology, 5, 01040. https://doi.org/0.3389/fpsyg.2014.01040
Shaffer, F., Meehan, Z. M., & Zerr, C. L. (2020).
A critical review of ultra-short-term heart rate variability norms research.
Frontiers in Neuroscience, 14, 594880. https://doi.org/10.3389/fnins.2020.594880
Stern, R. M., Ray, W. J., & Quigley, K. S. (2001).
Psychophysiological
recording (2nd ed.). Oxford University Press.
Tétreault, P., Mansour, A., Vachon-Pressau, E., Schnitzer, T. J., Apkarian, A. V., & Baliki, M. N. (2016).
Brain connectivity predicts placebo response across chronic pain trials.
PLoS Biology, 14(10), e1002570. https://dx.doi.org/10.1371/journal.pbio.1002570
Thompson, M. (2005). Intentions, empathy, and theory of mind:
Implications for personality and psychotherapy. Presentation to the
Annual Meeting of the American Association for the Advancement of
Science (AAAS).
Tortora, G. J., & Derrickson, B. H. (2021).
Principles of anatomy and
physiology (16th ed.)
. John Wiley & Sons, Inc.
Tracey, K. J. (2007). Physiology and immunology of the cholinergic anti-inflammatory pathway.
Journal of Clinical Investigation, 117(2), 289-296. PMID: 17273548
White, C., & Lammy, D. (2004). Infrared hand temperature mapping [Abstract].
Applied Psychophysiology and Biofeedback, 29(4), 306.
Wickramasekera, I. A. (1988).
Clinical behavioral medicine: Some concepts
and procedures. Plenum Press.
Wilson, J. (2003).
Biological foundations of human behavior. Wadsworth/Thompson Learning.