Relaxation
What You Will Learn in This Unit
Have you ever wondered why a walk in the park leaves you feeling refreshed, while sitting in traffic ties your stomach in knots? This unit explores the science behind relaxation and why developing relaxation skills is essential for both clinicians and clients in biofeedback practice. You will discover that relaxation, meditation, and mindfulness are overlapping practices that form a larger family of techniques, each with unique physiological and psychological effects.
Along the way, you will learn to separate fact from fiction by examining common myths about relaxation, including the misconception that relaxation is like deep sleep or that you must force yourself to relax. You will explore two theoretical road maps for understanding how relaxation works: self-stressing theory, which explains how we perpetuate our own stress responses, and psychological relaxation theory, which identifies 25 distinct relaxation states organized into six levels of depth.
A central theme throughout this unit is the distinction between biofeedback and relaxation. Although many people conflate these terms, biofeedback is simply information about your body's performance, while relaxation refers to specific practices that reduce physiological and psychological arousal. When clinicians combine these approaches through biofeedback-assisted relaxation training, they create a powerful synergy where biofeedback guides and reinforces relaxation practice, and relaxation helps clients transfer self-regulation skills to their daily lives.
You will also learn the difference between deep relaxation procedures like autogenic training, progressive muscle relaxation, and meditation, and abbreviated relaxation techniques like the Quieting Response. Each type serves a different purpose: deep relaxation creates a template for how relaxation feels and may help reset physiological setpoints, while abbreviated procedures help clients generalize their skills to real-world settings where they spend most of their time.
This unit covers the Relaxation/Meditation/Mindfulness construct, Biofeedback versus Relaxation, Biofeedback-Assisted Relaxation Training, the Many Pathways to Relaxation, Relaxation Myths, Two Road Maps for Self-Relaxation, Procedures That Produce Deep and Moderate Relaxation, Autogenic Training, Progressive Relaxation, Visualization, Meditation, Hypnosis, the Quieting Response, Nutrition, Hydration, and Physical Exercise.
BCIA Blueprint Coverage: This unit addresses Relaxation methods: Procedures, indications and contraindications (VII-B), and The effects of exercise on mood, physiological functioning, and presenting symptoms (VII-F).
Relaxation, Meditation, and Mindfulness
Smith (2021) views relaxation as a component of a more expansive relaxation/meditation/mindfulness (RMM) construct. Relaxation, meditation, and mindfulness overlap considerably, and understanding their relationship helps clinicians select appropriate interventions for their clients.
There is a bit of relaxation in all of meditation and mindfulness. There is a bit of meditation and mindfulness in all of relaxation. Nearly all texts and training programs teach blends of RMM. Although different techniques clearly have a different pattern of effects, all can be placed on the same psychological map. All can evoke experiences from the same lexicon (Smith, 2017, 2019; pp. 39-40).
Smith states that his definition is based on popular use, meaning relaxation is what most professionals call relaxation. Examples of relaxation exercises include autogenic training, paced breathing, progressive muscle relaxation, tai chi, visualization, and yoga (Smith, 1985, 1986, 1990, 1999, 2001, 2005, 2017, 2019).
For Smith, the core element of meditation is sustaining quiet, simple focus. Focused attention (FA) meditation (Lutz et al., 2015) concentrates on one stimulus, such as breathing sensations. Mindfulness meditation involves quietly attending to the flow of all stimuli, or a restricted domain of stimuli such as sounds, as a neutral observer.
Biofeedback Is Not Relaxation
Although consumers and clinicians sometimes conflate biofeedback with relaxation, they can be completely separate. Biofeedback is information about your body and its performance, nothing more and nothing less.
🎧 Listen to a Mini-Lecture on Biofeedback Is Not Relaxation
Biofeedback Is Not Inherently Relaxing
A high blood pressure reading (biofeedback) can be alarming rather than calming. The information itself does not produce relaxation; it simply tells you about your physiological state.

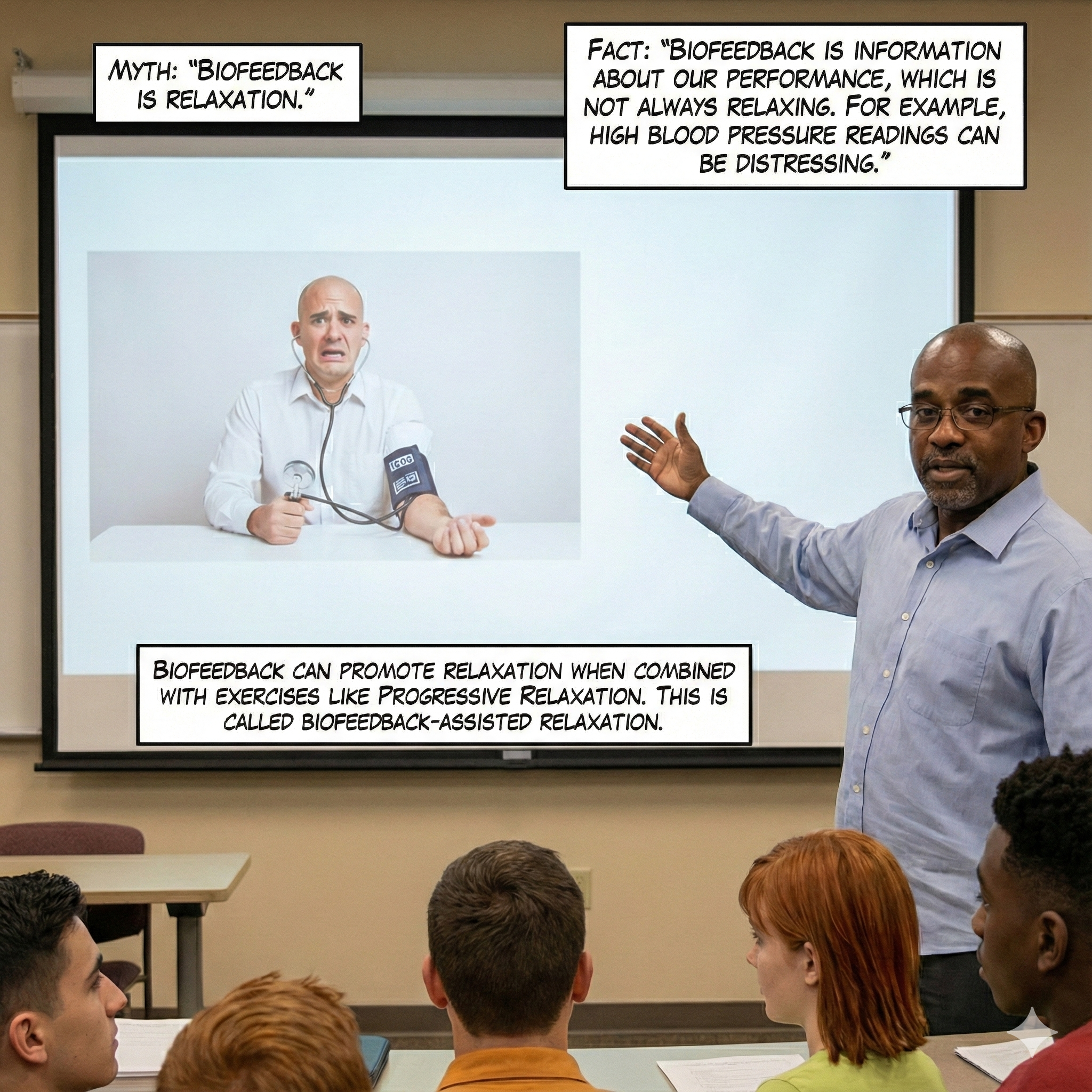
Biofeedback-Assisted Relaxation Training
In biofeedback-assisted relaxation training (BART), clinicians combine biofeedback with relaxation exercises to teach clients to relax. BART can use individual or combined biofeedback modalities to reinforce relaxation exercises like autogenics, guided imagery, mindfulness meditation, paced breathing, and progressive relaxation (Moss, 2020).
A high percentage of biofeedback treatment follows a stress-relaxation model, in which the purpose of biofeedback training is to cultivate a relaxed state and counteract the effects of chronic situational and personal stress (Moss, 2020).
The Many Pathways to Relaxation
Relaxation practices are remarkably diverse and vary in their degree of structure. An important clinical principle is to discover the relaxing activities your client already enjoys and build on them. The following examples illustrate the many ways people naturally find relaxation in their daily lives.
We can relax through structured exercises like meditation.

We can relax through expressive activities like hip-hop dance.

We can relax through exercise and participation in sports.

We can relax through prayer and meditation.

We can relax by immersing ourselves in nature.

We can learn a great deal about relaxation by watching our pets.

Play is an inherently fun way to disrupt the stress response and increase resilience. Children intuitively understand the value of play.

Urban teenagers can turn a cityscape into an obstacle course for parkour. See the World's Best Parkour and Freerunning on YouTube.

Finally, play can involve spending time with your best friend.

Relaxation Myths
Both clients and therapists share misconceptions about relaxation that can undermine treatment success. These myths include the beliefs that relaxation is like being deeply asleep, that all relaxation procedures produce the same relaxed state, that you must make yourself relax, and that brief versions of relaxation procedures are equivalent to the original methods. Correcting these misconceptions is crucial for effective treatment.
🎧 Listen to a Mini-Lecture on Relaxation MythsMyth: Relaxation Is Like Being Deeply Asleep
Relaxation training should teach clients to achieve a state of calm alertness instead of drowsiness. The goal is not to become sleepy or zoned out but to achieve a relaxed yet focused state. Relaxation practice should improve your performance when driving, presenting a talk, or hitting a golf ball, none of which would benefit from drowsiness.
Myth: All Relaxation Procedures Produce the Same Relaxed State
When we administer a psychophysiological profile to a new client, we often see some systems within normal limits and others one or more standard deviations outside clinical norms. Each client has a personalized response stereotypy, meaning a unique psychophysiological response pattern. For example, blood pressure and heart rate might be elevated while skin conductance level and upper trapezius muscle contraction are normal.
Mild and moderate stressors do not produce unidimensional physiological changes. Stressors will trigger changes in some systems but not others: blood pressure and heart rate may rise while skin conductance and upper trapezius EMG do not change. This illustrates the concept of response fractionation, in which body systems react independently to stressors. Stress responses are multidimensional.
If your client's response to stressors is unique and multidimensional, their response to a relaxation procedure will also be unique and multidimensional. For example, a progressive relaxation exercise focusing on forearm tension may lower blood pressure and heart rate without changing skin conductance or upper trapezius EMG. In contrast, a visualization exercise asking clients to imagine lying on warm sand may lower state anxiety without changing blood pressure, heart rate, skin conductance, or upper trapezius EMG. Relaxation procedures produce complex changes in each client; there is no generic relaxed state.
Myth: You Must Make Yourself Relax
A client's strategy during relaxation practice can result in clinical success or failure. When we introduce a relaxation exercise to lower blood pressure, clients should not practice it in a way that triggers vagal withdrawal, paradoxically raising their blood pressure.
Dr. Khazan explains why effortful self-regulation is self-defeating © Association for Applied Psychophysiology and Biofeedback.
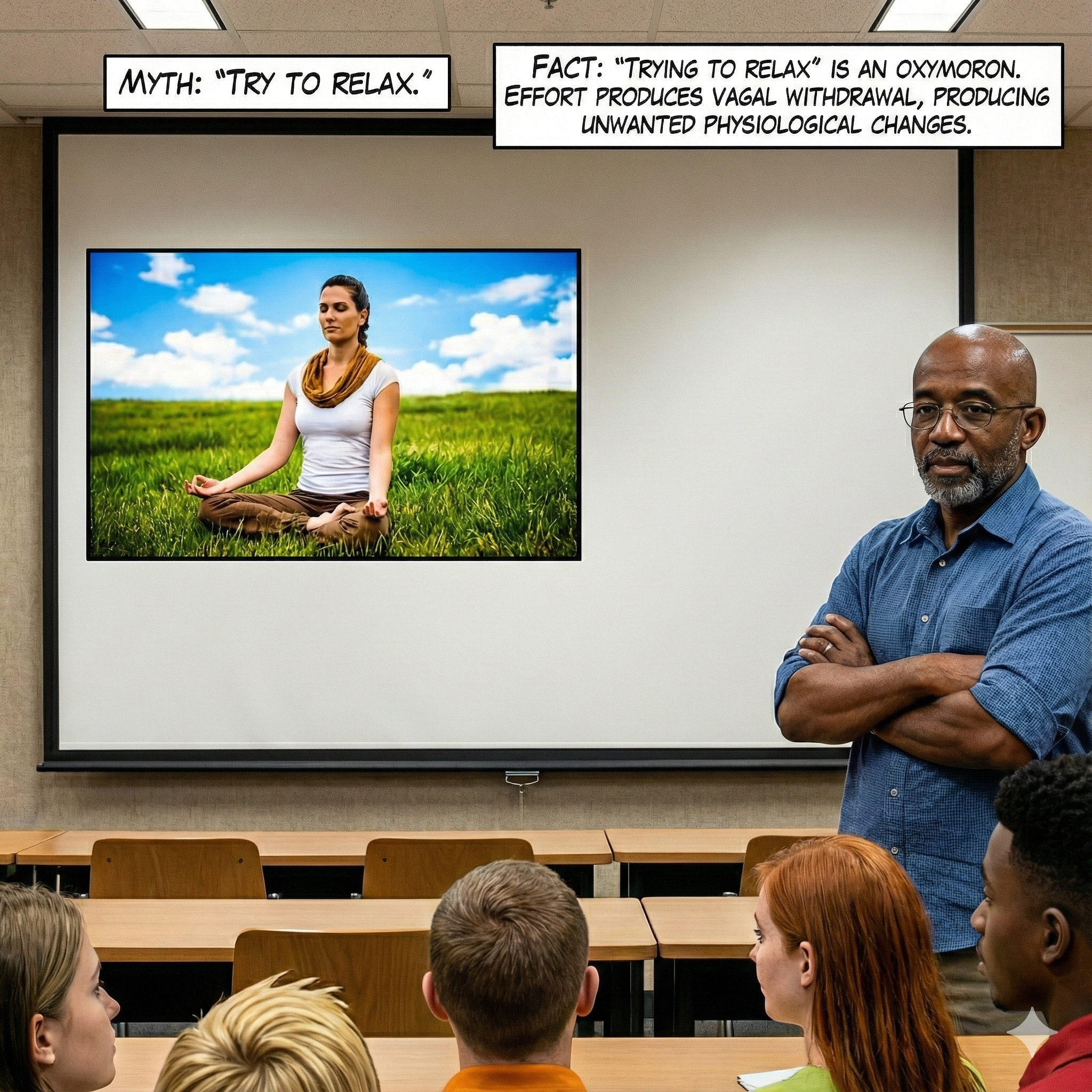
Although active volition, instructing muscles to contract, can play a valuable role in progressive muscle relaxation procedures, excessive effort can backfire. Shaffer et al. (2002) reported that high effort in autogenic training (AT) and progressive muscle relaxation (PMR) procedures caused unwanted physiological changes. Effort can trigger overbreathing and suppress the parasympathetic branch, producing vagal withdrawal (Khazan, 2019).
Therapists should remind their clients that relaxation is a state of calm alertness and that you cannot be calm when you force yourself to relax. Instead, therapists should encourage their clients to use passive volition, where they visualize a desired change and then allow their bodies to make the change at their own pace.
Myth: Abbreviated Versions Equal the Original Methods
Researchers often administer abbreviated versions of AT and PMR and then draw conclusions about the effectiveness of these techniques. They may leave out crucial elements of the original procedure, provide significantly less training time in session length and number of sessions, lack expertise in teaching the method, and play recorded relaxation instructions instead of offering live interactive training.
There are three issues with this approach. First, researchers should not be surprised when crippled versions of procedures originally taught over months or years do not produce the profound changes reported by their developers. Second, relaxation training success is greatly influenced by trainer skill and personality (Taub's "person effect"), just like athletic coaching success. Do not blame the tools. Third, recorded instructions have less impact than live instructions and cannot be adjusted to help clients overcome difficulties during a training session.
Two Road Maps for Self-Relaxation
Smith (2016) proposed two self-relaxation road maps that help explain how different relaxation techniques work: self-stressing theory and psychological relaxation theory.
Self-Stressing Theory
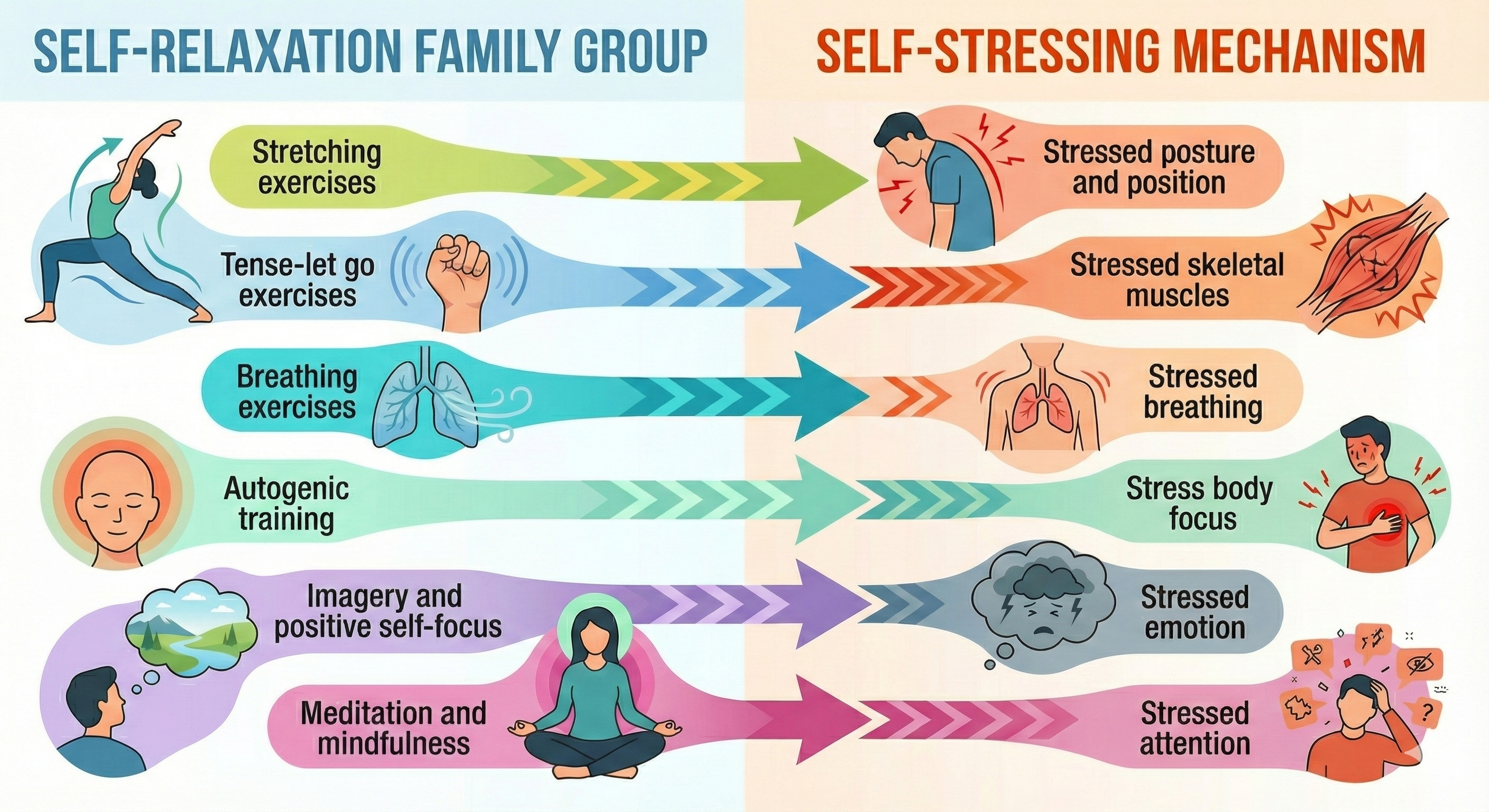
Self-stressing theory proposes that we initiate and perpetuate a fight-or-flight response in six ways: stressed posture and position, skeletal muscles, breathing, body focus (rapid breathing), emotion (anxiety), and attention (worrying about a threat).
Smith (2016) argued that the diverse self-relaxation strategies attempt to remedy these forms of self-stressing. A single family group may address more than one self-stressing mechanism. The table below shows how different relaxation technique families target different self-stressing mechanisms.
Psychological Relaxation Theory
Based on 31 published factor analytic studies and surveys of over 40 RMM techniques, Smith (2021) grouped 25 relaxation states (RMM states) into 6 levels. Several RMM exercises may produce the same subjective state. We recommend that professionals purchase Lehrer and Woolfolk's authoritative Principles and Practice of Stress Management (4th ed.) and read Smith's Overview of Stress and Stress Management in its entirety.
Smith characterized RMM theory this way:
My approach is not narrow-spectrum; it does not focus on a homogenous, static outcome state or trait (e.g., the relaxation response, focused awareness, or nonjudgmental acceptance). Instead, my approach is broad-spectrum and based on four ideas: (1) RMM has many defining effects, (2) these effects inform and influence each other, (3) they change over time, and (4) this change is not random or circular but evolves in a direction that is decreasingly self-referential and increasingly deep and encompassing. Simply, my broad-spectrum model is multidimensional, interactive, dynamic, and directional (for an elaboration, see Smith, 2017, 2019) (pp. 40-41).
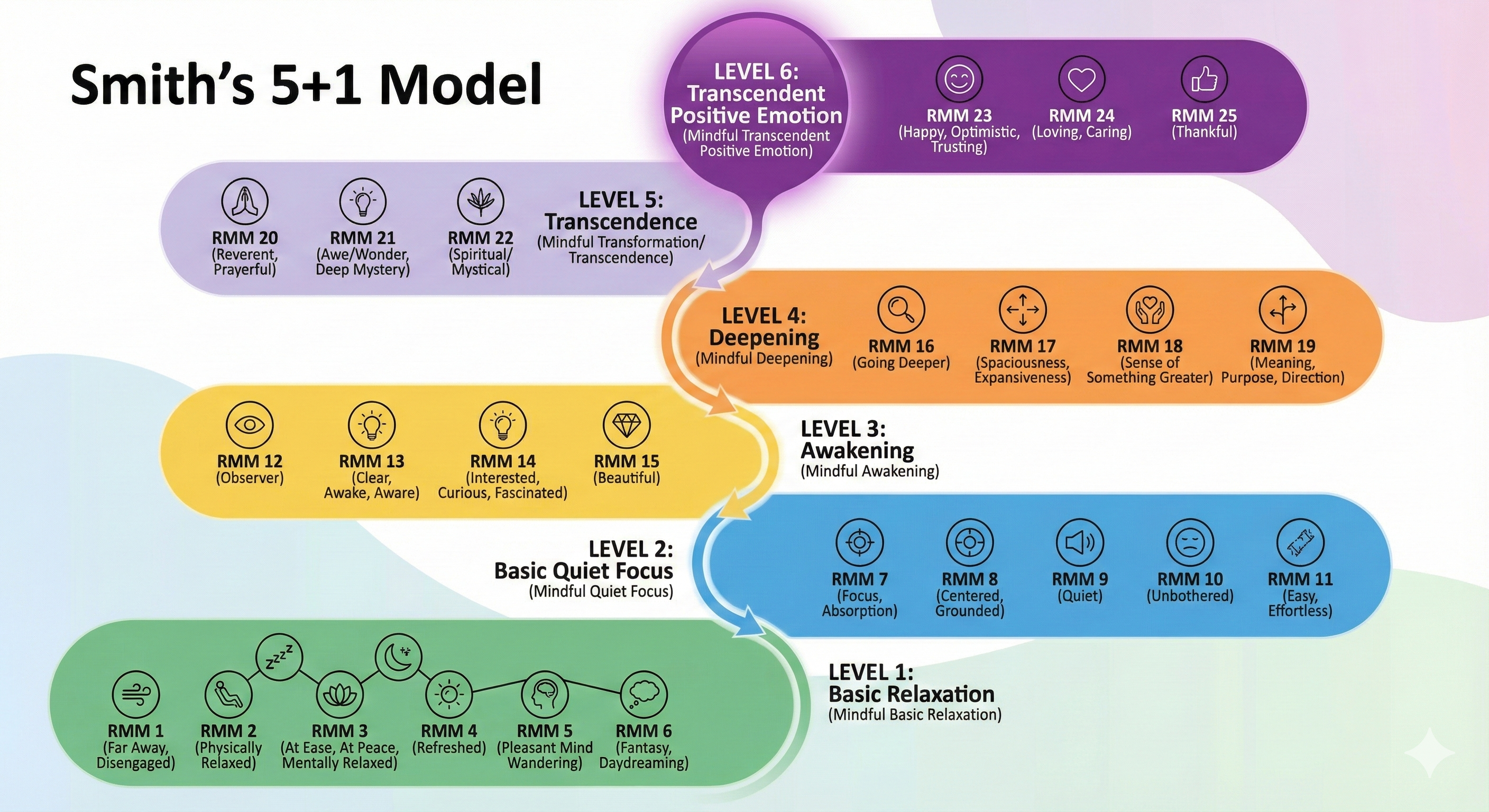
Smith (2021) argued that RMM states powerfully reinforce the initiation and maintenance of relaxation practice and are crucial to positive relaxation experiences. They enable clients to communicate their relaxation goals and experiences and incorporate relaxation into their daily lives.
Relaxation training combines deep relaxation and abbreviated relaxation procedures. We can categorize relaxation procedures in terms of subjective and physiological change, degree of sensory restriction, and length of practice.
🎧 Listen to a Mini-Lecture on Deep and Abbreviated Relaxation ProceduresAutogenic training (AT), progressive muscle relaxation (PMR), visualization, transcendental meditation (TM), clinically standardized meditation (CSM), and hypnosis can help clients achieve deep relaxation. They produce moderate-to-strong subjective and physiological changes, involve moderate-to-high sensory restriction, and are practiced for intermediate-to-long periods.
Abbreviated relaxation procedures like the Quieting Response (QR) produce mild-to-moderate subjective and physiological change, involve minimal sensory restriction, and are practiced for very brief periods.
Like throat-singing (shown below), deep relaxation exercises help clients experience profound relaxation, creating a template of how relaxation subjectively feels. This template guides relaxation practice and enables clients to first consciously, and later unconsciously, identify when they are distressed. When relaxation becomes automatic, clients may unconsciously detect their distress and unconsciously relax.

Deep relaxation exercises may help counter allostatic load and reset body setpoints for blood pressure, muscle contraction, and stress hormone levels. Finally, the belief that relaxation practice has been successful may increase your clients' perception of self-efficacy (personal effectiveness) and result in an internal shift in their locus of control (perceived cause of individual outcomes like health and illness).
These exercises may create a relaxation template, help clients develop an automatic relaxation response, help clients counter changes produced by distress and reset body setpoints, and increase perceived self-efficacy and internally shift their locus of control.
Abbreviated Relaxation and Transfer of Training
Abbreviated relaxation procedures help clients generalize relaxation skills to the settings outside of the clinic where they spend the most time (167 hours a week) and experience the most distress (commuting, home, and the workplace).

Generalization from a clinic to a client's environment, called transfer of training, is a critical hurdle in psychotherapy and relaxation training. Generalization is why you should practice abbreviated relaxation wherever you are, within reason.

Abbreviated relaxation procedures help clients transfer relaxation skills to their environment by making relaxation automatic. A stress response is a habit that has become automatic after months to decades of practice.
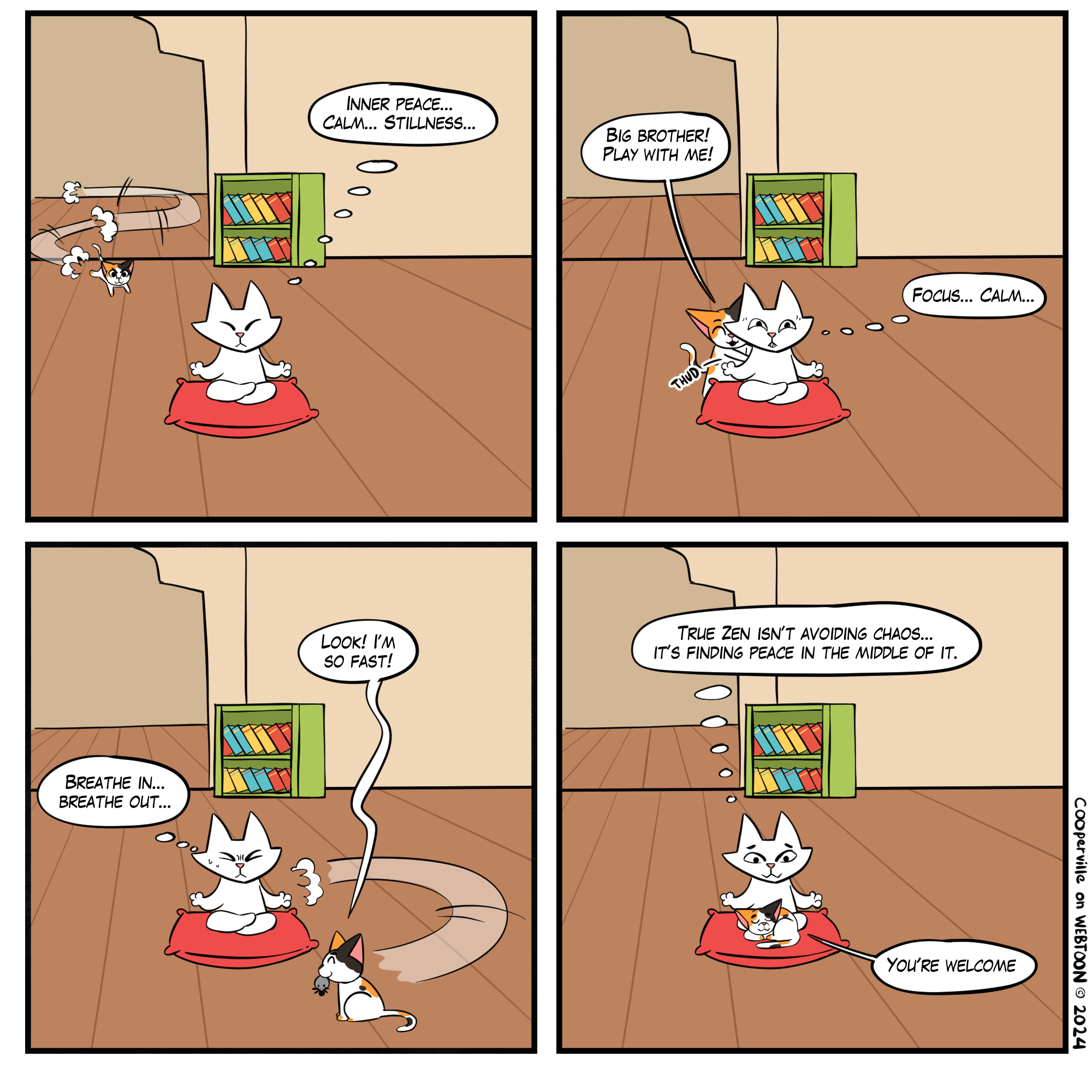
Although you should protect your initial relaxation practice from disruption by environmental stimuli (e.g., noise), generalization requires that you gradually expose yourself to mild distractions like TV, the calico kitten.
A relaxation skill is also a habit, but it is so new that its practice initially requires conscious supervision. The more clients practice a relaxation skill, the stronger this habit becomes. After about 6 months, clients may automatically replace a fight-or-flight response with relaxation when they encounter stressors (traffic slowdown). Abbreviated relaxation exercises may complement deep relaxation exercises in countering cumulative changes produced by distress. These exercises may also help reset body setpoints, increase perceived self-efficacy, and internally shift your clients' locus of control.
To summarize, abbreviated relaxation exercises may help clients transfer relaxation skills to their environment, develop an automatic relaxation response, counter changes produced by distress and reset body setpoints, and increase perceived self-efficacy and shift their locus of control internally.
The Relationship of Biofeedback to Relaxation Training
There can be a remarkable synergy between biofeedback and relaxation training. In BART, biofeedback helps clients refine their relaxation skills by guiding their practice with knowledge of results. Feedback immediately shows clients when relaxation strategies succeed or fail. Biofeedback provides objective, quantifiable evidence of performance success. Clients often trust physiological measurements more than their perception of improvement. Measurements in microvolts seem more real to them. This information can reassure clients that they have made progress, increase their motivation to practice, and help them continuously refine their relaxation skills.
Relaxation training, in turn, helps clients transfer self-regulation skills learned through biofeedback to their environment. Forty minutes a week of biofeedback training cannot change client stress responses by itself. These 40 minutes must counter the stressors encountered during about 10,000 waking minutes each week. Biofeedback training does not have a chance of changing clients' stress responses without weekly relaxation practice. Biofeedback research has consistently shown that successful clinical and performance outcomes require regular, but not daily, relaxation practice.
Autogenic Training
Johannes Schultz (1884-1970), a German neurologist and Nazi, developed AT during the 1920s based on clinical hypnosis research (Schaefgen, 1984). Schultz described clinical applications of AT to the Medical Society in 1926 and published his first book, Das Autogene Training, in 1932.
🎧 Listen to a Mini-Lecture on Autogenic Training and Progressive Relaxation
Schultz observed that deep relaxation and falling asleep are associated with sensations of limb heaviness and warmth. AT assumes that this process is bidirectional. Passively imagining heaviness and warmth can produce a deeply relaxed state. AT requires passive concentration, free of effort or goal direction.
Individuals also use passive concentration to perceive three-dimensional random-dot stereograms. To perceive a hidden image, they must allow their eyes to defocus until they see two patterns. At this point, an image will "jump out."

Luthe believed that visualization is crucial to achieving self-regulation in AT.
From Luthe's perspective, passive concentration reduces cortical interference with maintaining homeostasis by subcortical structures. The transition to a passive, pre-sleep, hypnagogic autogenic state is called autogenic shift. The challenge is to maintain the autogenic state without falling asleep. A client walks a tightrope between active attention and sleep (Luthe, 1979). Check BodyMindPower video Autogenic Training - A Guided Relaxation for a Deep and Restful Sleep.Autogenic Therapy
AT is a sequence of six standard exercises, autogenic modification, and autogenic meditation. Therapists often use complete or abbreviated versions of the standard exercises. They frequently dispense with autogenic modification and autogenic meditation. Training can be individual or in a group setting. The environment should be comfortable with minimal distraction. A client should sit or lie comfortably with good neck and leg support. The ideal position is lying supine on a couch since this minimizes muscle tension and promotes drowsiness. The room should be slightly darkened (Linden, 1990).Six Standard Exercises
The six standard exercises focus on physiological changes. A therapist prepares the client for the first exercise by reviewing its rationale, the learning process, common experiences, and the mechanics of autogenic training. Each standard exercise consists of a relaxation theme ("heaviness") a client subvocally repeats while visualizing that they are lying or sitting in a comfortable environment like a beach or a meadow (Schultz & Luthe, 1969). A passive attitude is the most crucial element. A relaxed position, conducive environment, and visualization are also important.AT consists of six relaxation themes.

AT's heaviness and warmth standard exercises (themes 1-2) are divided into seven parts.
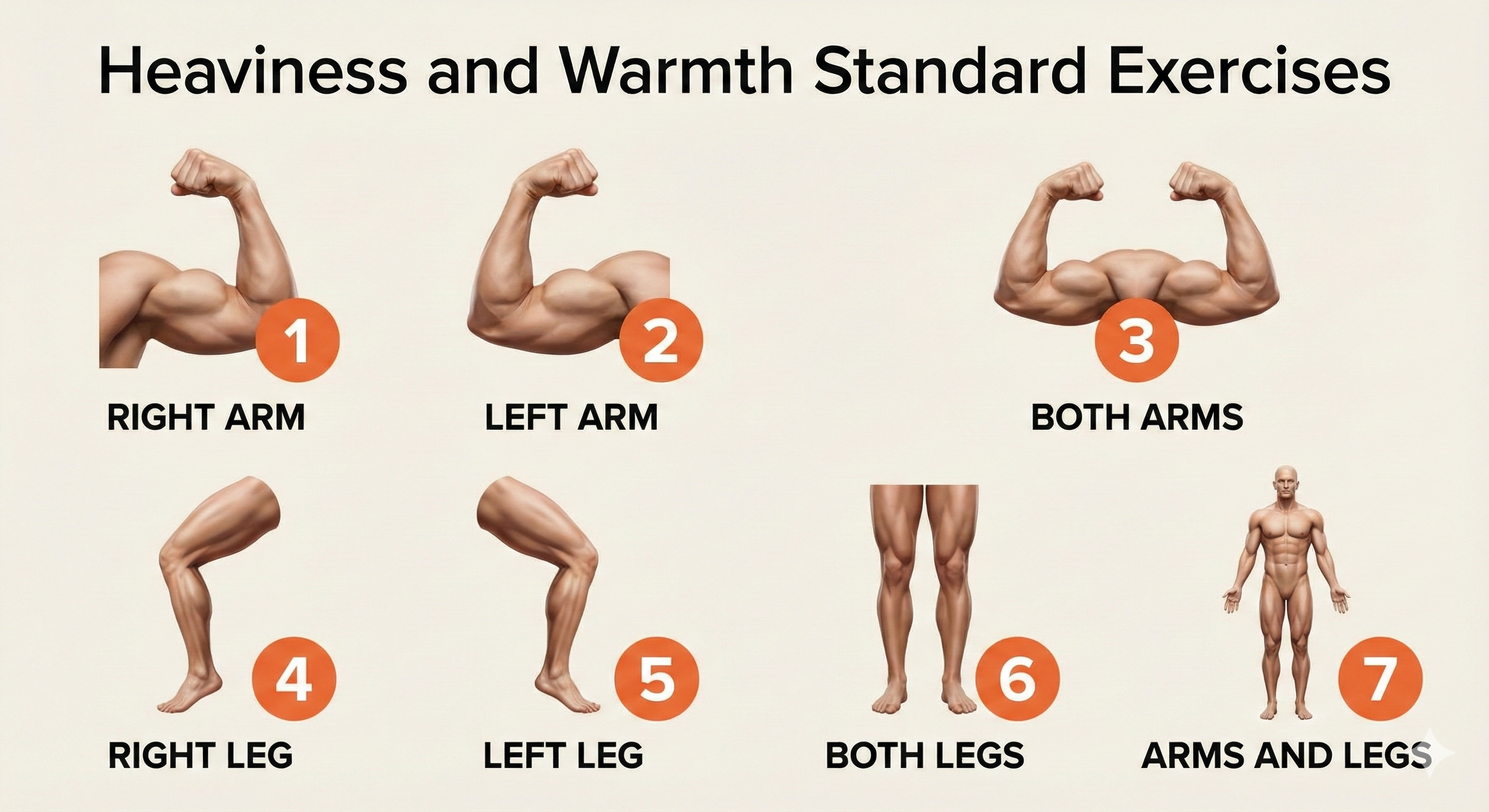
The remaining standard exercises (themes 3-6) consist of only one relaxation component. In total, the six standard exercises consist of 18 components. The European practice of 1-2 sessions per component requires almost 6 months to complete these exercises (Lichstein, 1988). American clinicians sharply abbreviate autogenic exercises (Pikoff, 1984), often providing less than one hour of training.
Each training session starts with the formula, "I am at peace." The initial practice may be as brief as 30 seconds per relaxation component (for a total of 9 minutes for one standard exercise). A client may extend performing a component to over 30 minutes as their skill increases. Standard exercises end with taking back procedures: vigorously flexing the arms, deep breathing, and opening the eyes: "Arms firm, breathe deeply, open eyes" (Linden, 1990).
Autogenic Modification
Autogenic modification procedures are used when a symptom like low back pain does not respond to the practice of the six standard exercises. Following a client's mastery of the standard exercises, a therapist may introduce organ-specific formulae or intentional formulae. Organ-specific formulae modify standard exercise themes (heaviness, warmth, calm and regular heartbeat, and coolness) to treat client symptoms ("My back is warm"). Intentional formulae, which may be reinforcing or neutralizing, increase or decrease behaviors. Reinforcing formulae motivate action ("I am energetic and will practice harder"). Neutralizing formulae reduce self-defeating statements ("My job frustration does not matter").Autogenic Meditation
Seven autogenic meditation exercises improve visual imagery skills after a client has mastered the six standard exercises. These exercises are designed to assist clients who find visualization hard. The exercise sequence is arranged in increasing difficulty. The client should follow the established order and only advance after mastering an exercise.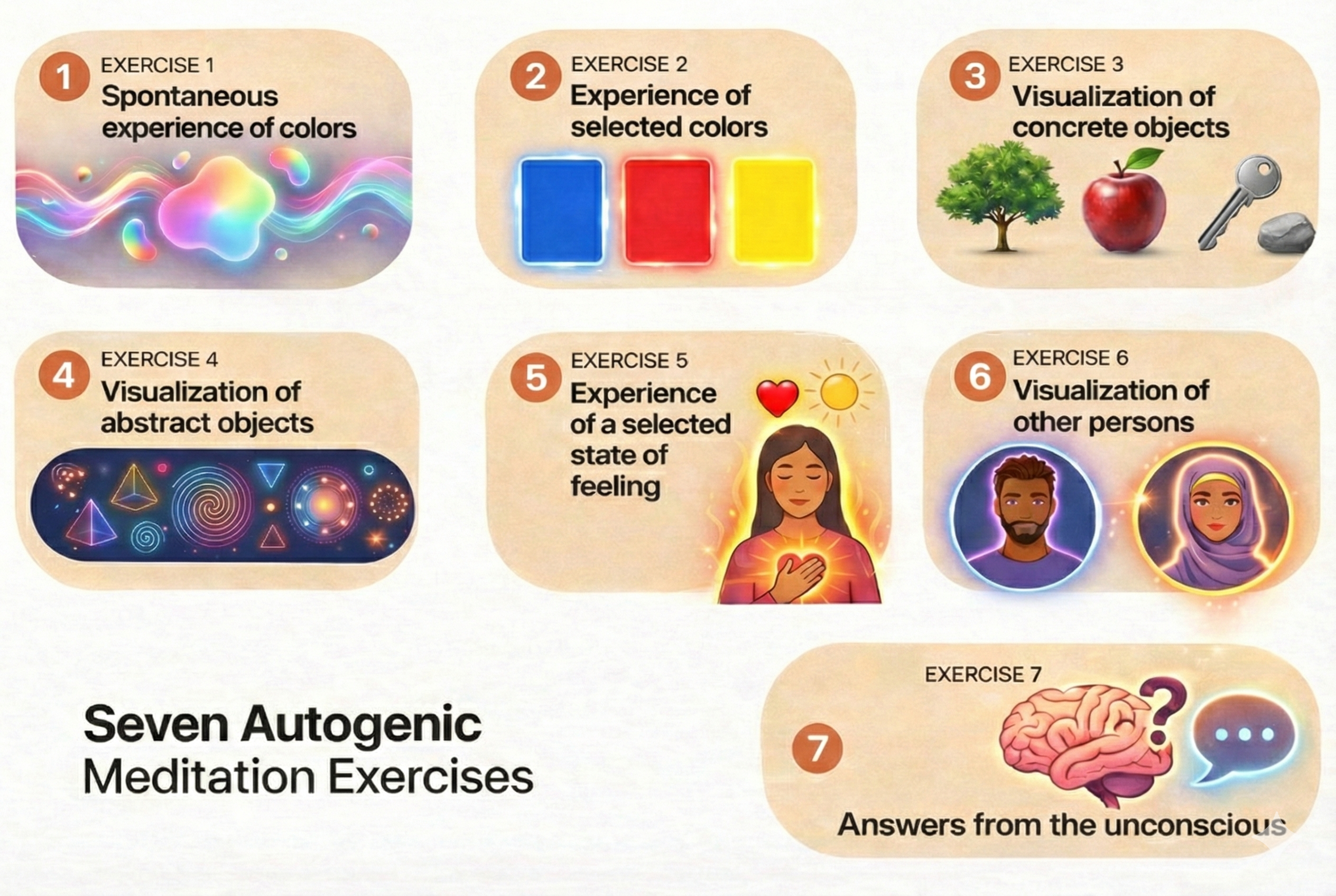
A client's visualization skills determine their rate of mastery. Moderate-ability clients may master all seven exercises in one or two sessions; others may require a month per exercise (Lichstein, 1988).
Physiological Effects
Eighty studies have demonstrated that autogenic training increases skin temperature and peripheral blood flow. Vasodilation becomes apparent during the "heaviness" phrases and increases during the "warmth" exercises. The temperature increases often followed the anatomical focus of the "warmth" exercises (Lichstein, 1988).These studies challenged Freedman and colleagues' (1983) conclusion that AT does not produce hand-warming. The authors assigned Raynaud's clients to listen to 3 minutes of tape-recorded instructions followed by the repetition of the phrase, "My hands are warm and heavy" for 13 minutes over 10 biweekly sessions. These clients did not increase their hand temperature.
Freedman and colleagues' conclusion was indefensible for two reasons. First, they did not use traditional AT. Instead, they used a crippled version that had failed to produce hand-warming in a previous study by Surwit and colleagues (1978). Second, their findings can't be generalized to all individuals since they were based on Raynaud's clients, who suffered from compromised peripheral blood flow.
AT Efficacy
Quantitative, meta-analytic findings indicated that AT was associated with medium-sized pre-to posttreatment effects ranging from d = 0.43 for biological indices of change to d = 0.58 for psychological indices in the Linden (1994) review, and d = 0.68 (biological indices) and d = 0.75 (psychological outcomes) in the Stetter and Kupper review (2002). The pooled effect size estimates hide considerable variability in behavioral/psychological effects for individual target problems; moderately sized improvements were reported for tension headache and migraine, hypertension, coronary heart disease rehabilitation, asthma, somatoform pain disorder, Raynaud's disease, and anxiety and sleep disorders (Linden, 2021, p. 546).
Recent research continues to support autogenic training's effectiveness across multiple conditions. A meta-analysis of 13 randomized controlled trials involving 576 participants with chronic pain found that AT produced a moderate, statistically significant reduction in pain intensity compared to passive control groups (g = 0.58), with no evidence of publication bias (Kohlert et al., 2022). These findings are particularly meaningful because AT allows pain patients to achieve relaxation without the additional muscle tension required by progressive muscle relaxation, making it gentler for those with musculoskeletal conditions.
A comprehensive 2023 narrative review examining AT's role in mental health identified 29 studies, including seven meta-analyses and systematic reviews, that explored AT's effects on mental disorders (Breznoscakova et al., 2023). The authors found consistent evidence for AT's efficacy in reducing anxiety across multiple studies and medium-range positive effects for mild-to-moderate depression. When used as an add-on intervention, a treatment combined with standard care or psychotherapy rather than used alone, AT showed particular promise for enhancing overall treatment outcomes.
Key Takeaways: Autogenic Training
Autogenic Training uses passive concentration and visualization to produce deep relaxation through sensations of heaviness and warmth. The six standard exercises can take months to master in the traditional European approach, though American clinicians typically abbreviate the training. Meta-analyses show medium-sized effects for both biological and psychological outcomes, with applications ranging from headaches to hypertension to sleep disorders. The key to success is a passive attitude, meaning allowing rather than forcing changes to occur.
Comprehension Questions: Autogenic Training
- Why is passive concentration essential to Autogenic Training, and how does it differ from active effort?
- What are the six relaxation themes in the standard AT exercises?
- When would a therapist use autogenic modification procedures instead of the standard exercises?
- Why was the Freedman et al. (1983) study's conclusion about AT ineffectiveness for hand-warming considered indefensible?
Progressive Relaxation
Edmund Jacobson (1888-1973) received training as a research physiologist and physician. Jacobson started using PMR in clinical cases about 1918 and published case histories in two 1920s articles (Jacobson, 1920, 1924). His most significant research productivity was between 1925 and 1940, when he studied the psychophysiology of progressive relaxation. During this period, he published the classic texts Progressive Relaxation (Jacobson, 1929) and You Must Relax (Jacobson, 1934).
PMR was not widely used until Wolpe incorporated an abbreviated version of this procedure in systematic desensitization. Wolpe designed this behavior therapy procedure to treat phobic disorders. Wolpe (1958) and Goldfried (1971) condensed Jacobson's standard procedure, which covered 50 muscle groups in 3-6 months of training. Wolpe's version trains about 15 muscle groups in 20 minutes (Lichstein, 1988).
Jacobson observed that clients maintain tension not required to perform a task (clenching teeth when writing a check) and are often unaware of that tension. He also discovered using electromyography that muscles usually do not relax even when we lie down. Jacobson theorized that unconscious muscle bracing wastes energy, disrupts performance, and produces stress disorders (Jacobson, 1929). He also asserted that anxiety is correlated with muscle tension, so muscle relaxation reduces anxiety.
Research has shown that the relationship between muscle tension, stress disorders, and anxiety is complex. Muscle tension may be a byproduct of an underlying disease instead of the cause (Suter, 1984).
Jacobson's original procedure trained clients to relax 2 or 3 muscle groups each session until 50 groups were trained. Several sessions might focus on a single difficult muscle group before moving to successive groups. Jacobson's approach was time-intensive, requiring 50-60 sessions in the clinic and 1-2 daily one-hour practice sessions (Suter, 1984). Studies do not show a difference in outcome between Jacobson's original PMR protocol and modern condensed versions (Snow, 1977; Turner, 1978).
In contrast to current protocols in which clients tense and relax muscle groups, Jacobson only asked clients to produce minimal muscle tension early in training. Jacobson's clients mainly employed passive relaxation in which they simply focused on muscle sensations (Lichstein, 1988). For Jacobson, the objectives of progressive relaxation were the development of muscle sense (awareness of muscle tension) and the reduction of useless residual tension. After eliminating residual tension, Jacobson encouraged his clients to develop differential relaxation skills, inhibiting unneeded muscle groups during routine activities. Check out the YouTube video Progressive Muscle Relaxation.
Popular PMR protocols are no more standardized than their autogenic counterparts. There are significant procedural differences (Lichstein, 1988). Watch the University of Toledo video Progressive Muscle Relaxation.
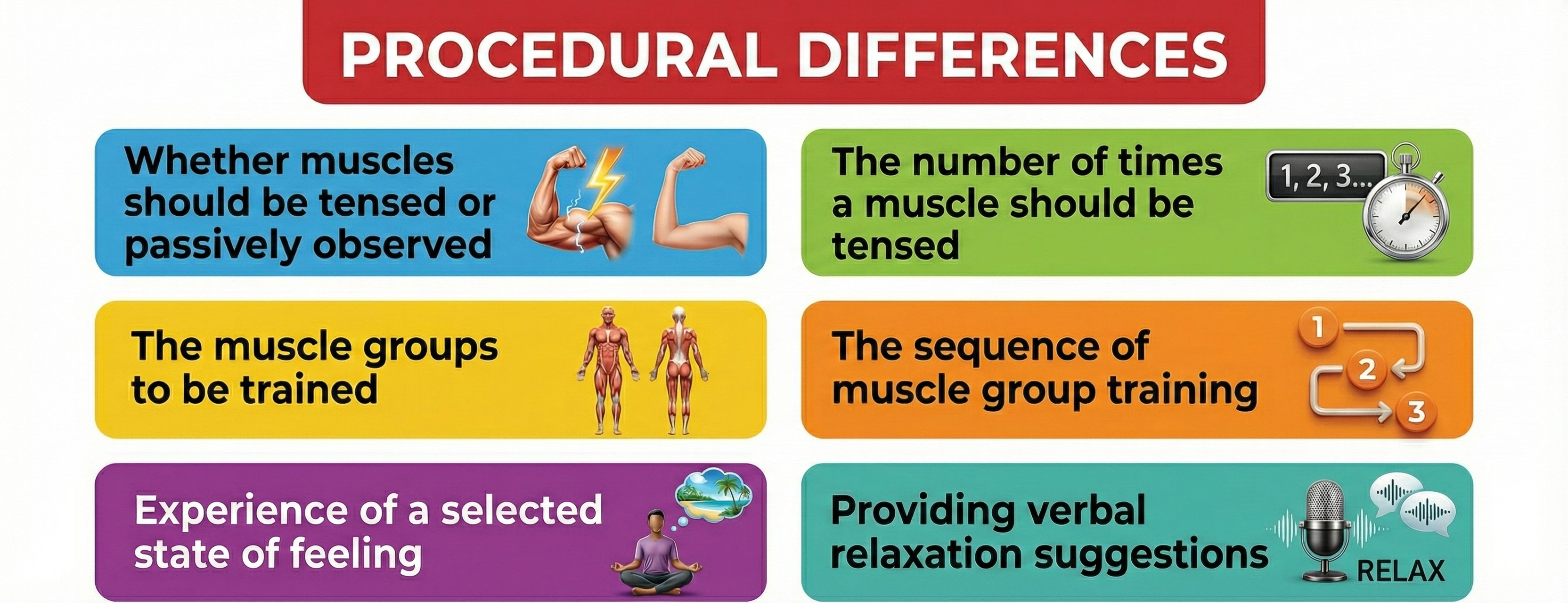
As in AT, clients may be trained individually or in groups. Also, a client reclines or sits in a slightly darkened room with eyes closed. For a conventional protocol covering 16 muscle groups, a client might tense for 7 seconds and relax for 45 seconds. The training sequence may be revised to accommodate a client's needs. Before training, a therapist should question each client to exclude already relaxed muscle groups and identify problem groups. Spastic or strained muscle groups may be skipped, or the tension level may be passively observed (without additional tensing). A therapist may repeat the tense-relax cycle two or three times for difficult muscle groups (Lichstein, 1988).
PMR Efficacy
Jacobson's clinical applications of progressive relaxation are impressive indeed. However, there apparently are no experimental (vs. clinical) data that validate the method, probably because of the extensive methodological difficulties in conducting an experiment...Although the literature on various forms of relaxation therapy is impressive, descriptions of the length and nature of training indicate either that the research has not used Jacobson’s progressive relaxation procedure or that this procedure has been confounded with other methods (McGuigan & Lehrer, 2021).
While Jacobson's original protocol remains understudied, the modified versions of progressive muscle relaxation widely used today have accumulated substantial empirical support. A comprehensive 2024 systematic review analyzed 46 publications from 16 countries covering more than 3,400 adult participants (Muhammad Khir et al., 2024). The authors found that PMR effectively reduces stress, anxiety, and depression in adults. When PMR was combined with other interventions like deep breathing or guided imagery, the combined techniques showed even greater efficacy, outperforming PMR used alone.
The COVID-19 pandemic provided an unfortunate natural laboratory for testing PMR's effectiveness under acute stress. A 2023 meta-analysis of studies involving 227 COVID-19 patients found that PMR interventions significantly reduced anxiety compared to usual care (Seid et al., 2023). The analysis also revealed improvements in depression scores and quality of life among patients receiving PMR. These findings suggest that PMR may be particularly valuable when individuals face high-stress situations where pharmacological interventions are complicated by other treatments or health conditions.
Visualization
Kenneth Pelletier's (1977) classic text Mind as Healer, Mind as Slayer proposed that mental imagery can produce harmful or beneficial physiological changes. Negative imagery can increase blood pressure, heart rate, muscle contraction, and pain.
Visualization, in which a client generates mental imagery that can be somatosensory and visual, is a common element in interventions ranging from autogenic training to behavior therapy. The vivid images created during visualization can help relaxation (standard autogenic exercises), prepare an individual to cope with stressful situations (mental rehearsal), and reduce symptoms such as anxiety, back pain, headache, hypertension, and ulcers. There are marked individual differences in visualization ability, and this capacity may overlap with hypnotic susceptibility. High-hypnotizable individuals who are gifted visualizers may achieve the best results using this strategy (Moss, 2004). Watch the University of Houston at Clear Lake White Cloud Visualization video.
Recent systematic reviews have strengthened the evidence base for visualization techniques. A 2024 systematic review of nine randomized controlled trials examined the effects of guided imagery, a structured form of visualization in which a practitioner or recording directs the client through a specific imagined scenario, on patients facing surgery (Kouhpayeh et al., 2024). The review found that guided imagery significantly reduced perioperative anxiety compared to standard care alone. This is particularly valuable in medical settings where pharmacological anxiolytics may interfere with anesthesia or recovery protocols.
Technology is also transforming how clinicians deliver visualization-based interventions. A 2024 pilot randomized controlled trial compared traditional guided imagery delivered by a practitioner with immersive virtual reality (IVR) guided imagery, where clients wear headsets that display relaxing 360-degree environments (Pardini et al., 2024). Among 72 participants, the VR condition produced substantially larger reductions in state anxiety (d = 2.45) compared to traditional guided imagery. While this technology is still emerging, it suggests that enhanced sensory immersion may amplify the therapeutic effects of visualization for some clients.
Meditation
Meditation is a family of disciplines that teach individuals to alter their consciousness for diverse outcomes, ranging from increased mindfulness to union with the divine. The meditative procedures reviewed in this section come from religious traditions like Hinduism (Transcendental Meditation) and secular practice (Benson's Relaxation Response, and Clinically Standardized Meditation). Graphic © Anatoli Styf/Shutterstock.com.
Transcendental Meditation (TM)
Transcendental meditation (TM) is a form of mantric meditation in which an individual repeats Sanskrit syllables that have been assigned by an instructor based on age or personality.
Benson (1975) identified four components that TM shares with other deep relaxation procedures: a "quiet environment, mental device, passive attitude, and comfortable position" (pp. 112-113). Benson developed a secularized version of TM, called the Relaxation Response, that incorporated these four elements and recommended that clients practice 1-2 times daily for 10-20 minutes. Watch the Relaxation Response: Dr. Herbert Benson Teaches You The Basics video.
Early TM hypertension studies lacked control groups, involved single-group pre-test-post-test designs, and yielded mixed results. Controlled trials of Benson's meditative procedure have not demonstrated clinically significant blood pressure changes in hypertensive individuals (Lichstein, 1988). Check out the 5 min Mantra Meditation for Beginners - Easy Guided Meditation.

Clinically Standardized Meditation (CSM)
Clinically standardized meditation (CSM) is a systematic secular meditative procedure incorporating components from meditative techniques like TM. A meditator selects or creates a mantra (soothing sound), repeats it aloud with the instructor and then alone, whispers it, and then mentally (silently) repeats it with eyes closed. Both the instructor and trainee meditate seated with eyes closed for 10 minutes, after which the trainee gradually returns to ordinary consciousness over 1-2 minutes. An instructor answers the student's questions about using this meditative technique and then instructs them to meditate alone for a specified period (10-20 minutes) after the instructor leaves the room. The student completes a questionnaire following meditation which is reviewed with the instructor. Then the instructor teaches the following week's meditative exercise and reviews how to control negative side effects. Meditation practice is prescribed twice daily for about 20 minutes and may be shortened if the student experiences adverse side effects (Lehrer & Carrington, 2003).Mantric Meditation Efficacy
Several meta-analyses of the data have been reported (Ooi, Giovino, & Pak, 2017; Park & Han, 2017; Shi et al., 2017), and these reviews generally confirm the earlier findings that mantra meditation is of decided value for health and emotional stability. These studies frequently call for more rigor in the design of studies and ask for larger samples. This is sound advice, except for the fact that funding for research on meditation is not easy to come by due to its seemingly esoteric nature, which still marks it as somewhat outside of the commonly accepted parameters. For this reason, research funds for more elaborate studies may not be readily obtainable. Hopefully, adequate support will bring forth such larger studies in the future.
PTSD is a notoriously difficult area to study due to the difficulties in pinning down the diagnosis and acquiring a suitable population for study, for follow-up, and for obtaining reliable outcome measures. Despite such difficulties, however, the general conclusion that mantra meditation can be highly effective in the treatment of many components of PTSD has been repeatedly confirmed (Kang et al., 2018; Metcalf et al, 2016; Cushing & Braun, 2018; Lang et al., 2012; Park & Han, 2017; Harne & Hiwale, 2018), and anxiety remains a major area in which mantra meditation seems to offer considerable clinical help (Cooney Roxbury, 2018; Travis et al., 2018) (Carrington & Lehrer, 2021, p. 403).
Mindfulness Interventions
Mindfulness is "preverbal awareness of the present moment with acceptance" (Germer, 2009). Clinicians have developed a family of mindfulness interventions over four decades, including Acceptance and Commitment Therapy (ACT), Dialectical Behavior Therapy (DBT), and Mindfulness-Based Stress Reduction (Khazan, 2019). These interventions teach clients to be in the moment without action or judgment. Mindfulness is not relaxation but can enhance relaxation training as clients nonjudgmentally experience emotions, physical sensations, and thoughts. Check out the Comfort Care Mindfulness Meditation video.Physical Changes
Lazar and colleagues (2005) used magnetic resonance imaging (MRI) to compare the thickness of the prefrontal cortex and right anterior insula in Buddhist Insight meditators and matched nonmeditators. They found that meditators had greater prefrontal cortical gray matter volume than the controls. This difference was greatest for older meditators and suggested that meditation may protect aging brains from apoptosis. Prefrontal cortex and right anterior insula volumes were positively correlated with years of meditation.A systematic review (Gard et al., 2014) of 12 studies, including 6 randomized controlled trials, concluded that various types of meditation might protect against age-related cognitive decline.
Hölzel and colleagues' (2009) used MRI to measure gray matter changes in the amygdala. The investigators randomized participants to an 8-week mindfulness-based stress reduction (MBSR) intervention or a wait-list control condition. They measured amygdala volume and perceived stress scale (PSS) scores before and after the intervention. Participants who received MBSR training reported significant stress reductions correlated positively with decreased right basolateral amygdala gray matter volume.
However, Kral et al. (2022) conducted an RCT that failed to replicate whole-brain or region-of-interest structural changes previously reported for an 8-week mindfulness-based stress reduction (MBSR) course in 218 meditation-naive participants. The authors highlighted the low statistical power of previous studies with sample sizes of 20 or less.
Mindfulness-Based Intervention (MBI) Efficacy
By mid-2013, a meta-analysis of MBIs drew on 209 studies (Khoury, Lecomte, Fortin, et al., 2013), showing comparable effects of MBIs to CBT and psychopharmacology and greater effects in comparison to other control conditions. Other meta-analyses are now showing effects for stress reduction in healthy individuals (Khoury, Sharma, Rush, & Fournier, 2015), in primary care (Demarzo et al., 2015), in older adults (Hazlett-Stevens, Singer, & Chong, 2018), and in the prison population (Shonin, Van Gordon, Slade, & Griffiths, 2013). An inclusive meta-analysis of psychiatric disorders (Goldberg, Tucker, Greene, Davidson, et al., 2018) examined efficacy by five types of control groups (from wait-list to evidence-based intervention), finding significant improved value both immediately after intervention and at follow-up for most comparisons, with MBIs being com-parable to evidence-based alternatives. There are now enough meta-analyses in core areas for a meta-analysis of the meta-analytic studies (Gotink et al., 2015). With the focus primarily on MBSR and MBCT, results show significant improvement in depressive symptoms, anxiety, stress, quality of life, and general physical functioning (Kristeller, 2021, p. 423).
More recent research has particularly focused on university students, a population at heightened risk for mental health difficulties. A 2024 GRADE-assessed systematic review and meta-analysis of 29 randomized controlled trials examined the effects of MBSR among university students (Pan et al., 2024). The analysis found significant reductions in anxiety (SMD = -0.29), depression (SMD = -0.32), and perceived stress (SMD = -0.41). Subgroup analyses revealed a positive relationship between intervention duration and improvements in negative emotions, suggesting that longer MBSR programs may produce greater benefits.
Military veterans represent another population with distinctive mental health needs. A 2024 systematic review and meta-analysis of 13 studies involving 1,131 veterans examined the effectiveness of MBSR for depression and PTSD (Li et al., 2024). Both within-group and between-group comparisons showed reductions in depressive and PTSD symptoms with medium effect sizes following MBSR intervention. Importantly, treatment effects were maintained at follow-up assessments for depression and mindfulness outcomes, suggesting durable benefits. The authors noted that MBSR may offer veterans a complementary approach to traditional trauma-focused therapies.
Hypnosis
The American Psychological Association's Division of Psychological Hypnosis cautions that hypnosis "is not a type of therapy" but instead "a procedure that can be used to facilitate therapy" (Kirsch et al., 1999, p. 3). Instead of hypnotherapy, which connotes an independent treatment like cognitive behavior therapy (CBT), we should use the term "hypnotically-assisted psychotherapy" (Moss, 2004, p. 37).Listen to Dr. Don Moss' Hypnosis, Mind-Body Perspectives, and Consciousness presentation.
Researchers disagree on the clinical efficacy and nature of hypnosis.
Barber (1996) views hypnosis as an altered state of consciousness and contends that analgesia involves negative hallucination where normal perception is suppressed. Hilgard (1978) hypothesized that the process of hypnotic induction produces an altered state of consciousness in susceptible individuals that allows them to create physiological changes. Barber (1982) conceptualizes hypnosis as a trait or relatively permanent predisposition to respond to suggestion and believes that the hypnotic process is not simply relaxation. He challenges the need for hypnotic induction (promotion of a hypnotic state) and argues that individuals respond equally well to suggestions without a trance state. Most hypnotherapists agree that all hypnotic procedures involve self-hypnosis (self-suggestion).
Hypnotic suggestibility (responsiveness to suggestion) was measured originally by instruments like the Stanford Hypnotic Susceptibility Scale and the Harvard Group Scale of Hypnotic Susceptibility. Clinicians can administer the recent Elkins Hypnotizability Scale more briefly than the hour required for the Stanford and Harvard scales while achieving relatively strong concurrent validity with the older scales (Kekecs et al., 2016).
Moss and Willmarth (2019) described hypnotic ability as a relatively stable trait when measured over a lifetime. A study of monozygotic and dizygotic twins estimated that hypnotic susceptibility has a heritability index of 0.64 (Morgan, 1973). A heritability index estimates the percentage of variation due to genetic influences. Values close to 1.0 indicate strong genetic influence.
A 25-year longitudinal study (Piccione et al., 1989) reported test/re-test correlations of 0.64, 0.82, and 0.71 for measurements at 10, 15, and 25 years, respectively.
The distribution of this trait in the population is relatively normal, which means that there are individuals with very low and very high hypnotic ability. Moss and Willmarth (2019) caution that about 20% of patients may be poor candidates for medical hypnosis applications due to low hypnotic ability. Interventions to increase suggestibility do not help most of these individuals (Lynn et al., 2015). For this reason, therapists should measure client suggestibility to determine whether to use a hypnotic procedure.
The Role for Biofeedback
Hypnosis can be effectively combined with biofeedback/neurotherapy (Moss, 2004). Wickramasekera (2003) proposed different roles for biofeedback with highly hypnotizable and medium-to-low hypnotizable individuals. He argued that highly hypnotizable clients will best respond to hypnotic procedures and that biofeedback can help illustrate the connection between mind and body. In contrast, medium-to-low hypnotizable clients are often better candidates for more intensive biofeedback training, which may increase their hypnotic susceptibility.The Promise of Hypnosis in Integrative Healthcare
Most patients show moderate-to-high hypnotic ability and achieve comparable outcomes to validated medical interventions. Moss and Willmarth (2019) advocate inclusion of adjunctive hypnosis in integrative healthcare programs where its addition enhances treatment outcomes.For this to happen, it is critical that the patient's complaint be one for which there is a strong research base supporting the value of hypnotic treatment. There is good research support for the application of hypnosis for anxiety disorders, depression (including major depression), post-traumatic stress disorder, stress management, sleep disorders, smoking cessation, weight management and eating disorders, and the addictions. There is also strong research support for the use of hypnosis for acute and chronic pain, IBS, colitis, diabetes mellitus, hypertension, skin conditions including psoriasis, chemotherapy induced nausea, and pediatric problems such as anxiety, school phobia, and recurrent abdominal pain (Elkins, 2017; Nash & Barnier, 2008). (p. 500)
Hypnosis for Chronic Pain
Hypnotic treatment is more effective than placebo in producing analgesia (insensitivity to pain) in highly suggestible clients (Jacobs et al., 1995). However, clients with low suggestibility respond to analgesic suggestions at the same rate as they respond to placebos (Miller et al., 1991). While researchers disagree about the mechanisms responsible for hypnotic analgesia, there is convincing clinical evidence that hypnosis can effectively treat acute and chronic pain.
A meta-analysis (Montgomery et al., 2000) revealed that analgesic suggestions reduced pain in about 75% of subjects and comparably reduced clinical and experimental pain. Hypnotic procedures have been successfully used in burn pain, cancer pain in children, childbirth discomfort, dental pain, headache, low back pain, pain from sickle cell disease, and surgical pain. These techniques are underutilized due to misconceptions such as "hypnotized clients are unaware of their surroundings" (Brannon, Feist, & Updegraff, 2022).
Moss and Willmarth (2019) summarized Patterson's review of hypnosis for chronic pain:
Similar to his table related to acute pain, Patterson (2010) presented a table related to chronic pain that included 14 controlled studies of hypnosis (12 randomized), in chronic conditions including fibromyalgia, headaches, cancer-related pain, back pain, and irritable bowel syndrome (IBS)-related pain. Again, all studies found that hypnosis was equal to or better than standard care treatments which included group support, biofeedback, medication, relaxation, Autogenic training, attention control and CBT. (p. 499)
Hypnosis for Surgical Patients
Moss and Willmarth summarized meta-analyses by Montgomery et al. (2002, 2007) on surgical applications of hypnosis.Montgomery et al. reviewed 20 well-controlled research studies, using meta analytic techniques, and concluded that hypnosis is an effective adjunctive treatment for patients undergoing surgery.
The meta-analysis showed a broad beneficial impact of hypnosis with surgical patients, across outcome categories. Subjective measures such as anxiety and pain, objective measures such as analgesia use, physiological measures, recovery time, and treatment time, all showed comparable beneficial outcomes for patients in the groups receiving hypnosis. The patients in the hypnosis groups showed better medical and psychological outcomes than 89% of the patients who did not receive hypnosis. Later research by Montgomery et al. (2007) showed that not only could hypnosis reduce patients suffering, enhance healing, and optimize recovery time, but that the savings to the hospital were substantial, mainly in reduced time in surgery. (pp. 499-500)
Hypnosis as an Adjunct to CBT for Stress
Clinicians do not have to choose between CBT and hypnosis. Kirsch et al. (1995) reported compelling evidence that hypnosis can improve CBT efficacy.The 18 studies that were analyzed in the Kirsch et al. (1995) report comprised 20 comparisons of hypnotic with nonhypnotic CBT groups, with a total of 90 effects and 577 participants. Larger positive effects tended to occur in larger samples. The average weighted effect was 0.66, so the average person receiving CBT in a hypnotic context did as well as the person at the 75th percentile or so of those receiving CBT without hypnosis.
Of these studies, Kirsch et al. (1995) identified 14 in which the only difference between hypnotic and nonhypnotic conditions was the use of the word hypnosis during relaxation instructions and training. The average weighted effect size for interventions labeled hypnotic, compared with the same intervention without the label hypnosis, for these 14 studies was d = 0.63. Thus labeling an intervention as hypnotic increases its efficacy by more than half a standard deviation (Karlin, p. 560).
Contemporary meta-analyses continue to support hypnosis as an effective intervention for pain management. A 2024 systematic review and meta-analysis of 70 studies involving over 6,000 participants examined hypnosis used adjunctively with other treatments for clinical pain (Jones et al., 2024). Hypnosis added to usual care produced small but significant additional analgesic effects for chronic pain, medical procedures, and burn wound care, with reductions of approximately 7-9 points on a 0-100 pain scale. These findings are particularly meaningful given that hypnosis carries minimal side effects compared to pharmacological alternatives.
A comprehensive 2023 umbrella review synthesized evidence from two decades of hypnosis meta-analyses across multiple health domains (Rosendahl et al., 2024). The authors found consistent evidence for hypnosis efficacy in acute pain, chronic pain, and several psychological conditions. Notably, hypnosis has achieved Level-I recommendation status from the North American Menopause Society for managing menopause-associated vasomotor symptoms, representing formal recognition of its evidence base. The review also found that adverse events in hypnosis trials are rare and typically mild, supporting its safety profile.
Key Takeaways: Hypnosis
Hypnosis is a procedure that facilitates therapy rather than a therapy itself. Hypnotic suggestibility is a relatively stable trait that varies across the population, with about 20% of people being poor candidates for hypnotic interventions. Research supports hypnosis for anxiety, depression, PTSD, pain management, and surgical preparation. Combining hypnosis with CBT can increase treatment efficacy by more than half a standard deviation. Biofeedback and hypnosis can work synergistically, with the optimal combination depending on the client's hypnotic ability.
Comprehension Questions: Hypnosis
- Why is hypnotic suggestibility important to assess before using hypnotic procedures?
- According to Wickramasekera, how should biofeedback be used differently with high vs. low hypnotizable clients?
- What evidence supports the effectiveness of hypnosis for chronic pain?
The Quieting Response
Stroebel developed the Quieting Response (QR) abbreviated relaxation exercise to counteract the fight-or-flight response.
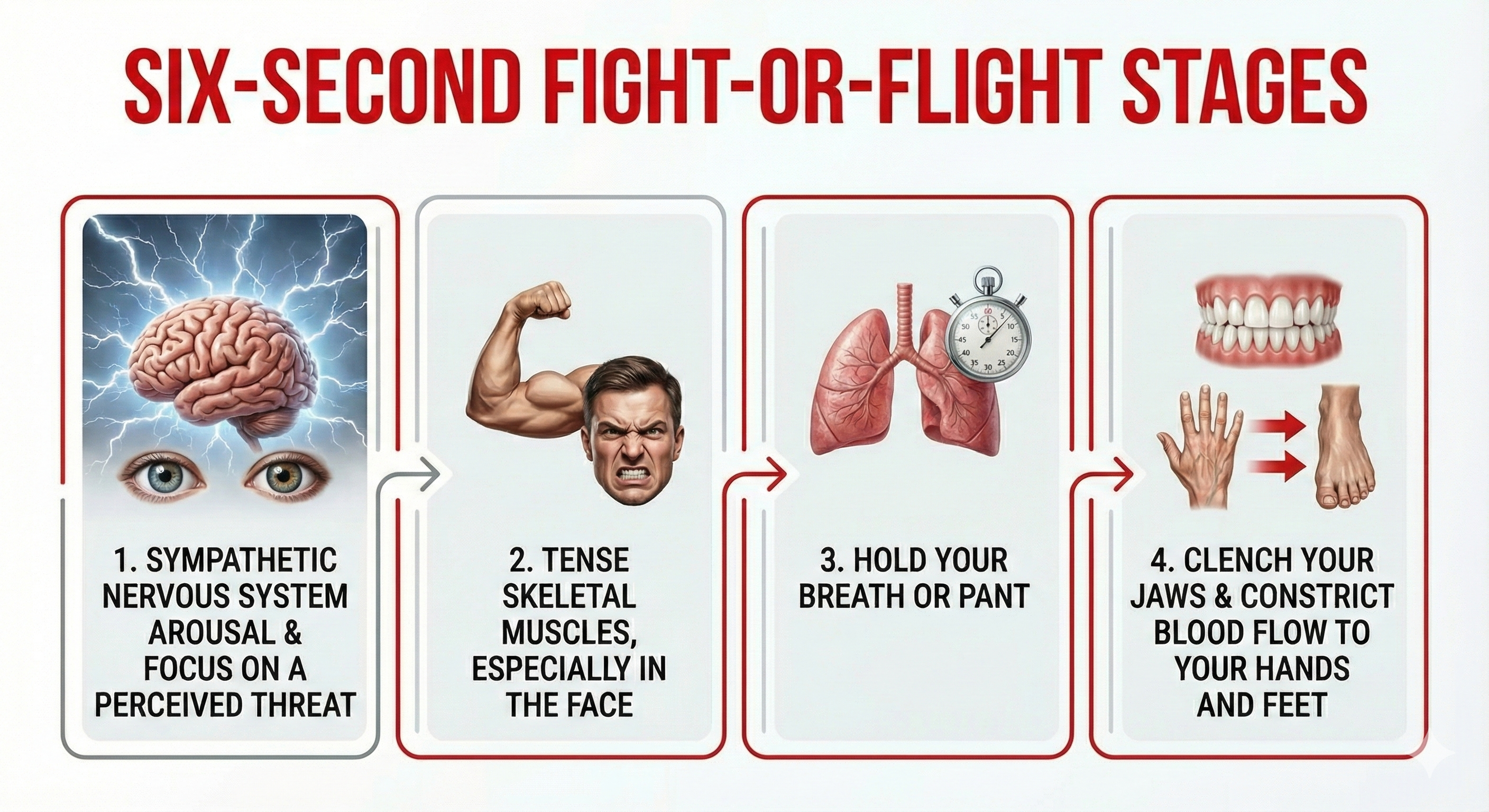
🎧 Listen to a Mini-Lecture on Chuck Stroebel's Quieting ResponseThe 6-second fight-or-flight response consists of four stages.

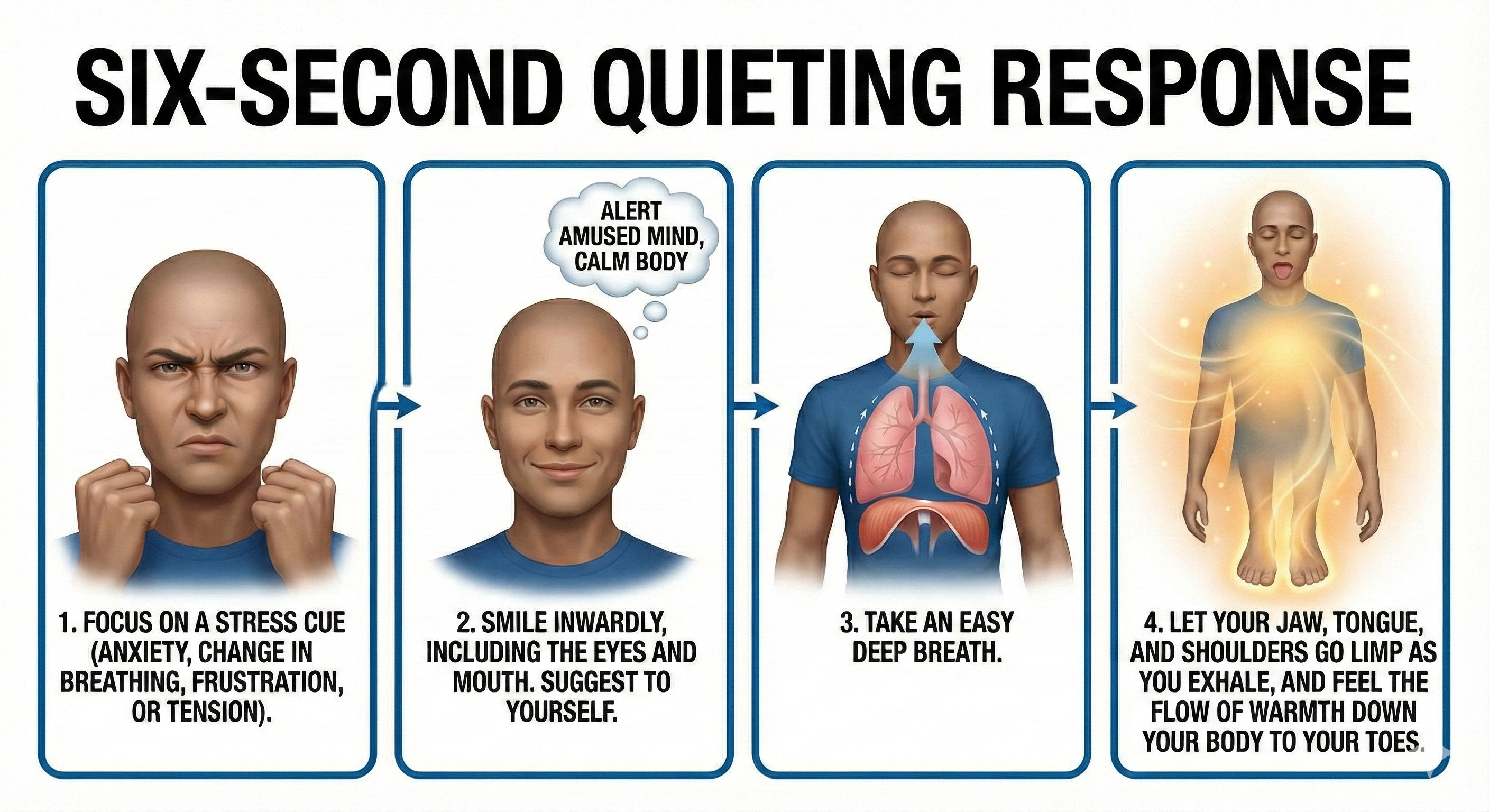
The 6-second QR consists of four corrective stages.
Stroebel recommended that clients learn the QR in eight learning sessions scheduled about one week apart. The activities for each session were described in QR: The Quieting Reflex (Stroebel, 1982). He advised clients to initially practice the QR whenever they experience annoyances, as many as 50-100 times a day. He cautioned that it would take about 6 months for the QR to become automatic. While 100-times-a-day practice might seem excessive, it only involves 600 seconds or 10 minutes per day. Stroebel estimated that 80% of clients practicing the QR achieve this level of proficiency and continue using this technique after two years.
Stroebel explained that the 80% compliance rate was due to the minimal time commitment required by the QR and the fact that clients do not have to disrupt daily activities to perform this 6-second exercise. "They controlled the technique; the technique did not control them." (p. 82)

Relaxation Training Issues
Causes of Deep Relaxation Training Failures
No one knows the average quality of instruction in AT and PMR when delivered as part of biofeedback training. There are many reasons that deep relaxation training fails.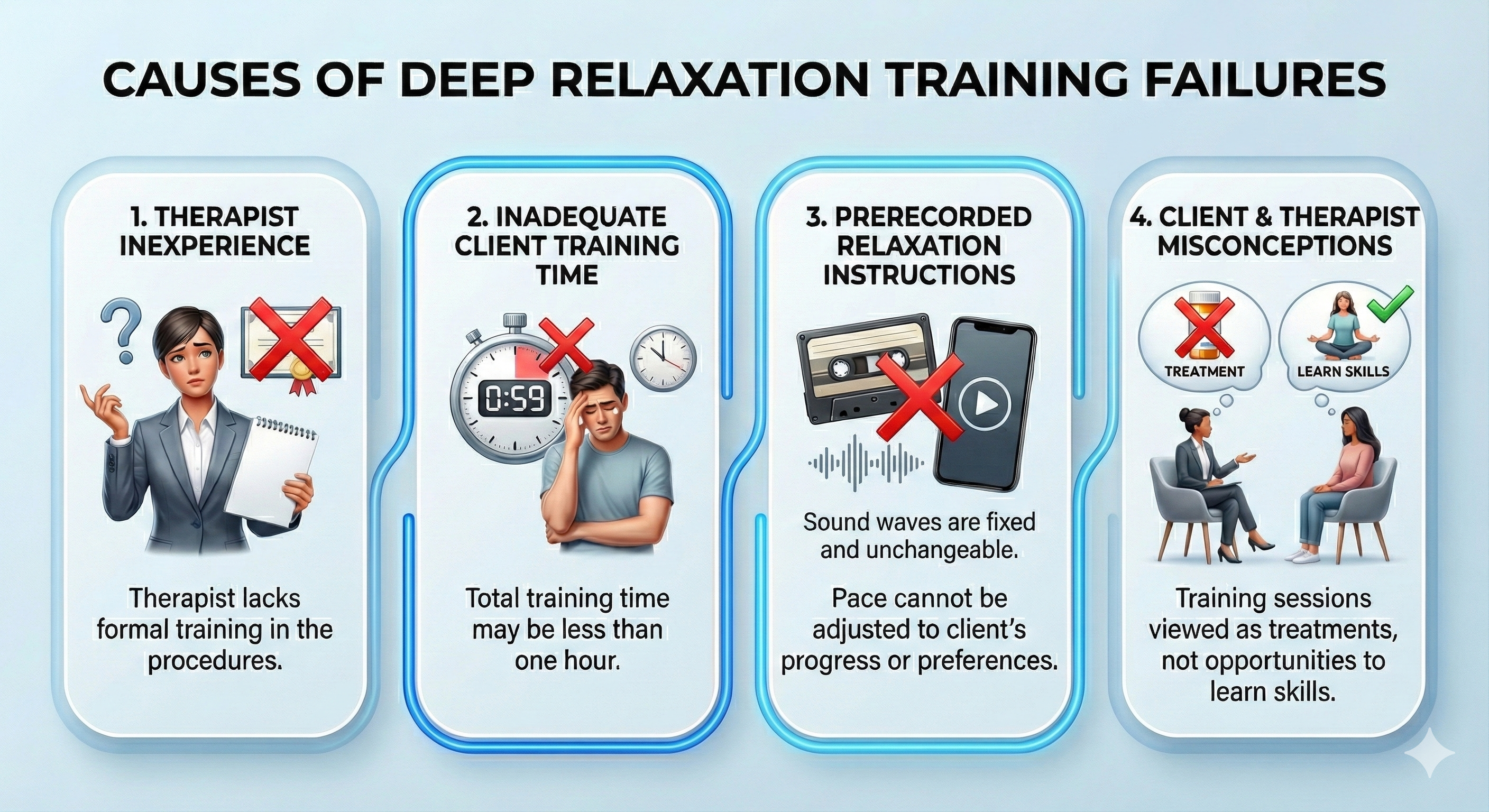
Recorded Relaxation Exercises
The professional can benefit from recorded relaxation exercises because they conserve training time, increase flexibility regarding when and where the client can practice, reduce the professional's burnout from the repeated presentation of relaxation scripts, and standardize relaxation script language.There are many practical benefits of recorded exercises. The cost of therapy may be lower due to fewer sessions. The therapist may schedule more clients. Therapist credibility and client enthusiasm may increase as the exercises produce desired results. Finally, client practice shortens the time to achieve mastery.
From a client's perspective, recorded exercises are desirable because they increase comprehension and retention, improve client satisfaction, motivation, and compliance, provide more consistent instructions and standardize exercises, provide information that family members can understand, allow for practice with fewer distractions, and help the client learn to pace relaxation exercises.
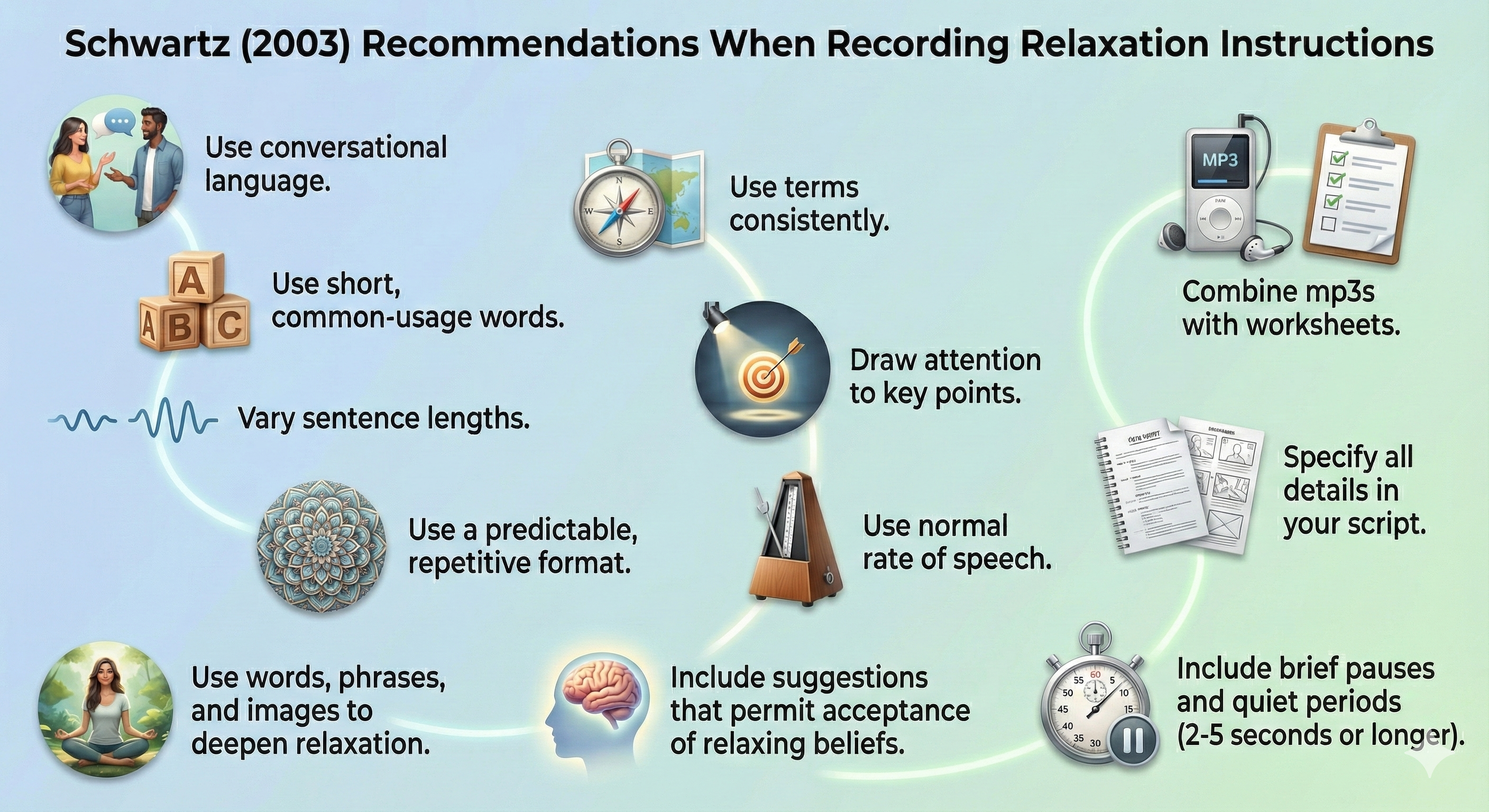
Schwartz (2003) recommended several steps when recording relaxation instruction.
Therapists should consider teaching clients to record exercises in their voices to increase client skills and promote an internal locus of control. We want clients to perceive relaxation as a skill they can refine through practice. We don't want them to use recordings as substitutes for medication. In Wickramasekera's language, we want to promote "skills, not pills."
Research suggests that live instructions may be more effective than taped instructions. A therapist's physical presence may produce more motivating demand characteristics than a recording. The advantage of live instructions may also be due to a therapist's ability to adjust relaxation training to the client's immediate experience and progress. For example, a therapist might suggest changes in sitting position or reduced effort during practice, observing psychophysiological measurements. Finally, a therapist can adjust pacing to an individual client's performance.
Negative Side Effects of Relaxation Training
Striefel (2004) cautioned that BART could produce negative reactions in any client.
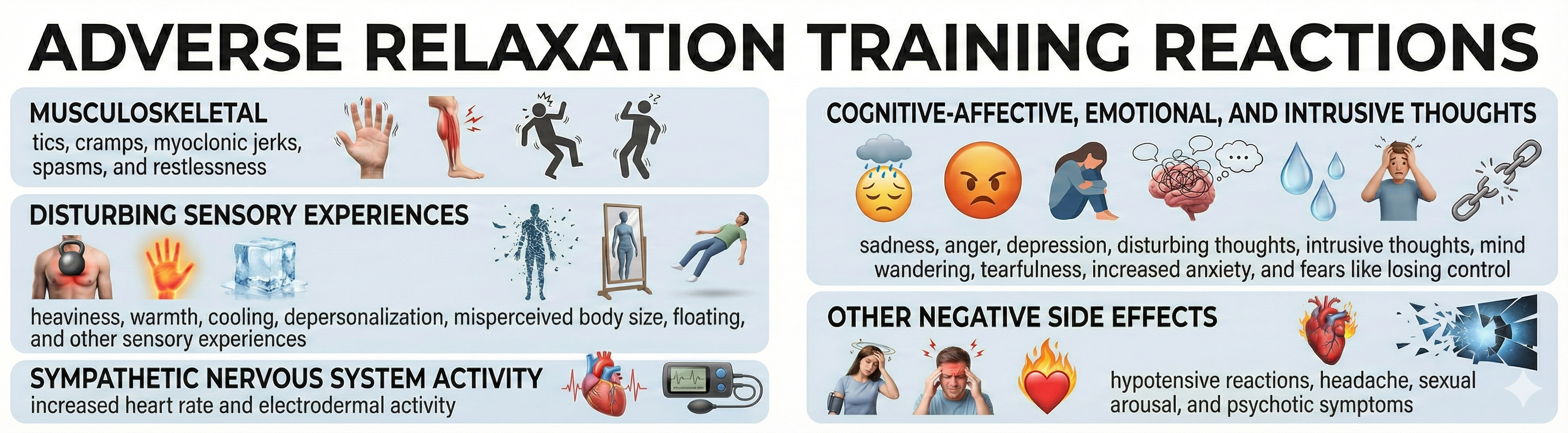
🎧 Listen to a Mini-Lecture on Negative Side Effects of RelaxationMost negative reactions to BART are due to its relaxation component.
While Budzynski (1994) suggested that a thorough psychological history can identify clients with an elevated risk of adverse reaction, therapists must be prepared to respond to problems in clients without diagnosed disorders.
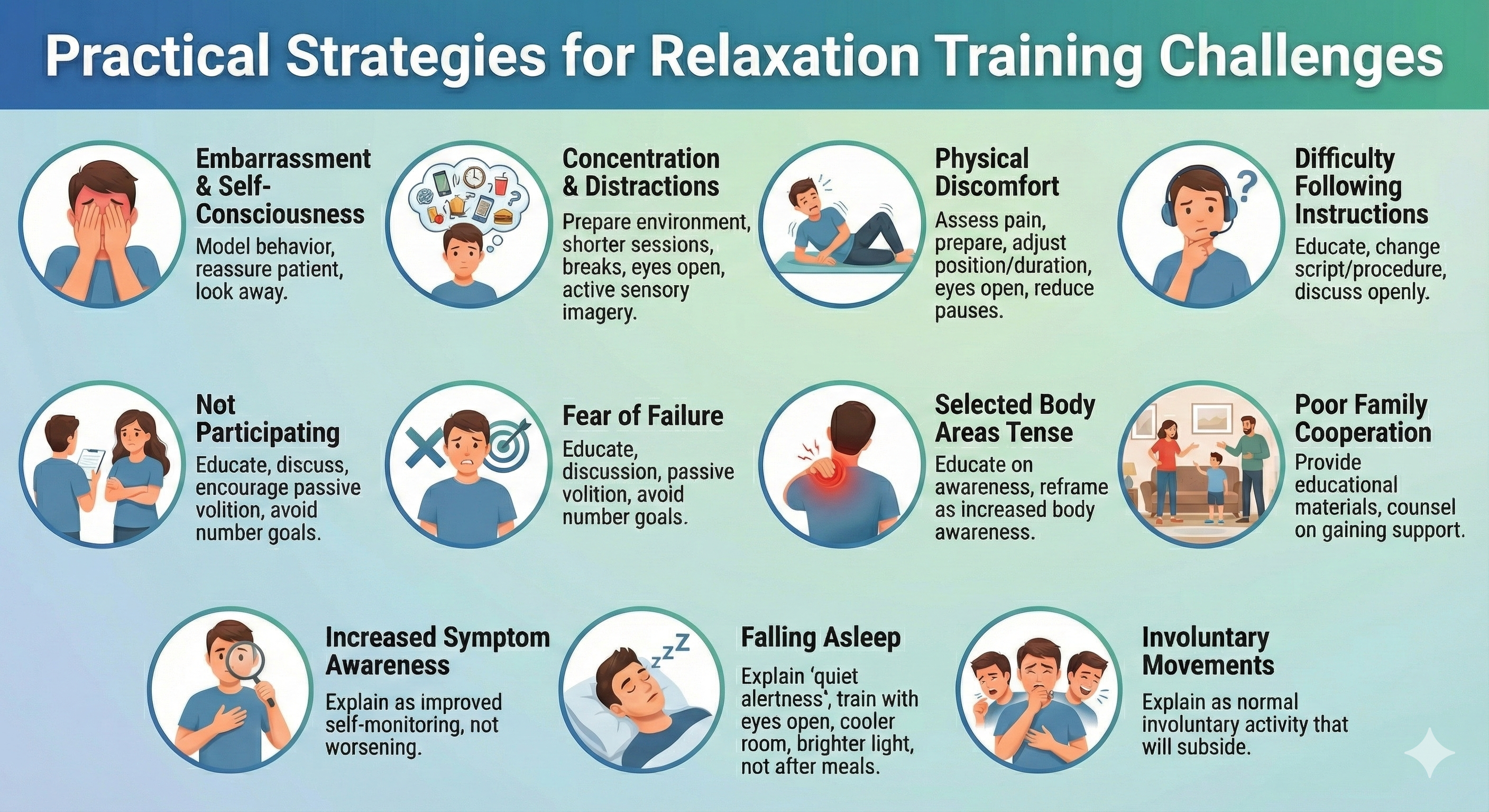
Schwartz, Schwartz, and Monastra (2016) advised that while significant severe adverse reactions are rare, mild-to-moderate adverse responses can interfere with training, possibly end promising therapy, and reduce client practice of assigned relaxation exercises.
When clients experience adverse reactions like anxiety, muscle spasms, tics, and increased sympathetic activation, a biofeedback therapist can reassure the individual and adjust biofeedback therapy and home practice assignments. In the rare case of a severe adverse reaction that exceeds the therapist's expertise, they may need to consult with or obtain supervision from a more experienced professional. If they cannot effectively treat their client, they may refer them to another clinician. Nash and colleagues (2001) contend that biofeedback therapists who are not licensed mental health professionals should not treat clients with a DSM diagnosis without licensed supervision.
Deep relaxation procedures like autogenic training and progressive relaxation can result in negative experiences.
Intrusive thoughts are among the most common adverse reactions to BART or relaxation exercises by themselves.

A survey by Edinger and Jacobsen (1982) of 116 psychologists who used a relaxation procedure revealed that relaxation side effects are common. For example, 15% reported intrusive thoughts, and 9% fear of losing control.
The adverse reactions experienced during relaxation training can be grouped as follows.

Physical Exercise

Physical exercise is crucial to psychophysiological health. While an hour of exercise per day may be optimal, physicians often recommend at least 30 minutes of moderate-intensity activity (brisk walking) at least 5 days per week or 20 minutes of high-intensity training (running) at least 3 days a week. The American College of Sports Medicine recommendations for four age groups are below (USDHHS, 2018). The table below was adapted from Brannon et al. (2022).

Exercise Health Benefits
Dozens of more recent studies have examined the relationship between physical activity and cardiovascular mortality. A systematic review of these studies shows that physical activity confers a 35% reduction in risk of death due to cardiovascular causes (Nocon et al., 2008). The same review concludes that physical activity confers a 33% reduction in risk of death due to all causes. Furthermore, both men and women benefit from physical activity, but risk reductions may be larger for women than for men (Nocon et al., 2008). More recent reviews confirm this link (Lavie et al. 2019; PAGAC, 2018). A dose-response relationship exists between levels of vigorous physical activity and reduced risk of all-cause mortality (Samitz et al., 2011), and a large reduction in risk appeared when comparing people who reported no activity to those who reported low levels of light-to-moderate physical activity (PAGAC, 2018; Woodcock et al., 2011). Thus, some activity is far better than none, but there are still benefits adding more activity to some activity (Brannon et al., 2022, p. 405.)
A landmark 2023 umbrella review synthesized 97 systematic reviews encompassing 1,039 trials and over 128,000 participants to examine exercise effects on mental health (Singh et al., 2023). Physical activity produced medium-sized reductions in depression (median effect size = -0.43), anxiety (-0.42), and psychological distress (-0.60) compared to usual care. The largest benefits occurred in people with diagnosed depression, HIV, kidney disease, and in pregnant and postpartum women. Higher intensity exercise was associated with greater symptom improvement, though shorter interventions paradoxically showed stronger effects than longer ones.
A 2024 network meta-analysis published in the British Medical Journal examined 218 randomized trials involving 14,170 participants with major depressive disorder to identify optimal exercise prescriptions (Noetel et al., 2024). Walking, jogging, yoga, strength training, and mixed aerobic exercise all showed larger reductions in depression than active controls, with effects comparable to or exceeding those of psychotherapy and antidepressants. Dance emerged as particularly effective for depression, while yoga showed the strongest benefits for anxiety. These findings support including exercise as a frontline treatment option alongside traditional interventions.
Physical exercise reduces mortality, increases life expectancy by an average of 2 years, and is associated with a lower risk of specific cancers (breast, colon, lung, prostate, and rectum), Type 2 diabetes, osteoporosis (decreased bone density), hypertension, cardiovascular disease, and stroke. Moderate physical activity can increase basal metabolism and help clients control their weight, reduce low-density lipoproteins (LDL), increase protective high-density lipoproteins (HDL), and possibly lower triglycerides. Watch the 10 Benefits Of Exercise On The Brain And Body video.Exerkines
Exerkines are molecules released by tissues like muscles and fat during exercise, and they play a big role in explaining why exercise is so good for our health (Khedkar, 2025). These molecules include proteins, hormones, and other compounds that send signals to nearby or distant cells in the body.For example, a molecule called interleukin-6 (IL-6), released by muscles, helps improve metabolism and energy production in cells, while another molecule, irisin, can boost brain function. Exerkines help with many things, like slowing aging, improving heart health, and even keeping skin healthy. Because these molecules work together in complex ways, it's hard to replicate all the benefits of exercise with a single drug.
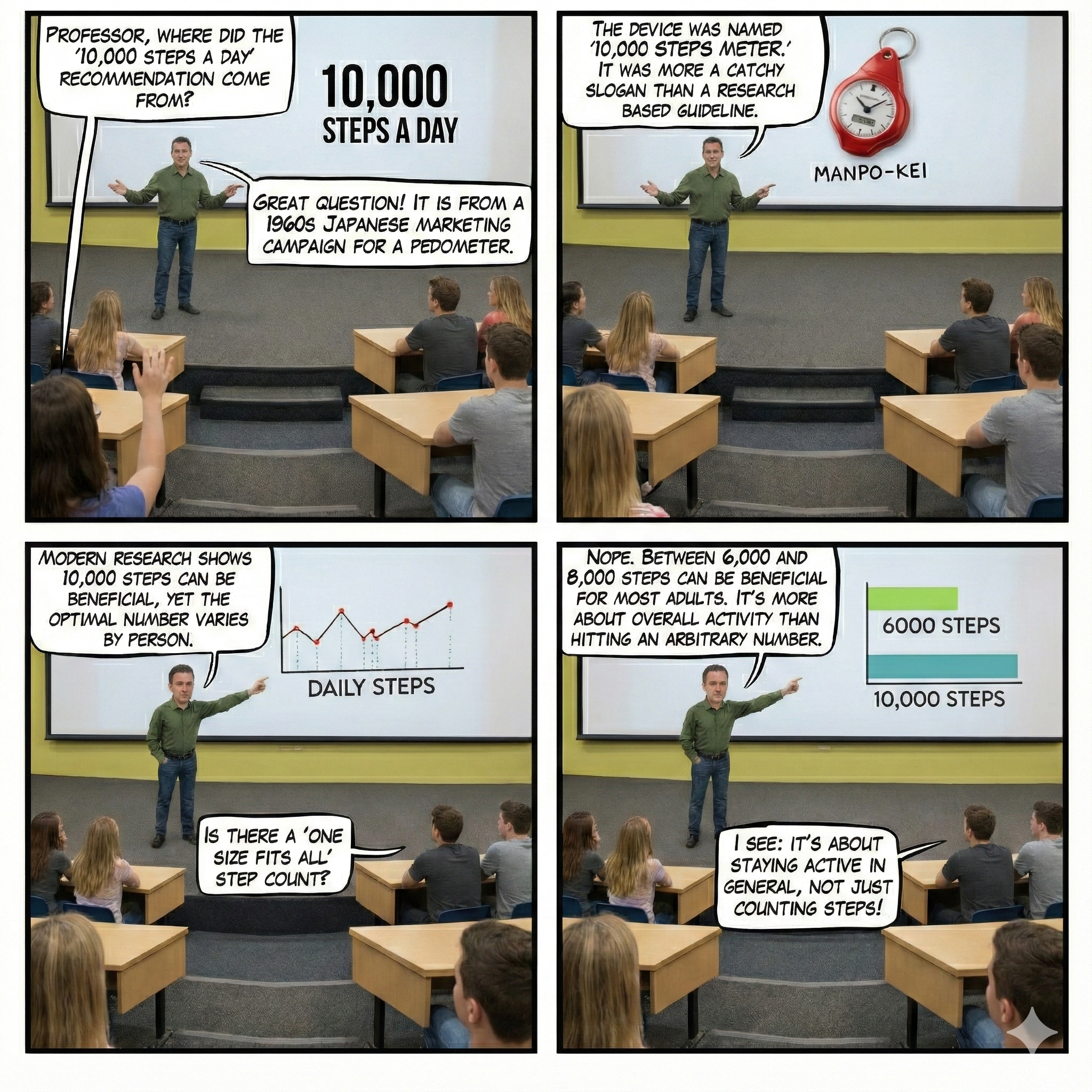
7,000 Steps
The 10,000-steps guideline originated in a Japanese pedometer marketing campaign. A prospective cohort study that followed 2100 adults on average for 10.8 years found that 7,000 steps were a mortality-risk dividing line. Participants who logged at least 7,000 steps experienced a 50-70% lower mortality risk than those who achieved less than 7,000 steps, regardless of step intensity (Paluch et al., 2021).
Nutrition

Acute and chronic stress disorders may deplete B-complex vitamins (50-100 mg/day), calcium (1,000 mg/day), and magnesium (400 mg/day), requiring their increased intake through dietary sources or supplements (University of Maryland Medical Center Complementary Medicine Program, 2005).
Clients should avoid or minimize caffeine consumption due to its activation of the sympathetic nervous system and potential to disrupt sleep. They should also restrict alcohol intake due to the risk of abuse and physical dependency, interaction with prescription medication, and potential interference with sleep. Check out the YouTube video Bill Nye The Science Guy & Nutrition.
Careful dietary choices can promote health (Taylor, 2015). A fiber-rich diet can reduce the risk of cardiovascular disease and obesity by lowering insulin levels (Ludwig et al., 1999). A diet high in beans, fish, fruits, poultry, vegetables, and whole grains and low in potatoes, processed and red meats, and refined grains can reduce vulnerability to coronary artery disease (Fung et al., 2001). Replace trans and saturated fats with polyunsaturated and monosaturated fats to improve heart health and reduce inflammation. Graphic © Mykola Komarovskyy/Shutterstock.com.

A healthy diet should keep saturated fat under 10% of your daily energy intake, restrict salt to less than 5 g, including 30-45 g of fiber, and two to three servings of fruits and vegetables per day. Fish, especially fish rich in omega-3 fatty acids like salmon, should be eaten one to two times a week. Finally, men should limit alcohol consumption to two standard drinks and women to one standard drink (Vaddadi, 2016). Graphic © Brian A. Jackson/Shutterstock.com.

Hydration
Well-hydrated adults are more likely to experience healthy aging than those who do not consume sufficient fluids. Serum sodium levels rise when fluid intake falls. The National Institutes of Health evaluated three decades of health data from 11,255 adults. Adults with high-normal serum sodium were more likely to experience chronic health conditions, age more quickly, and die earlier than those with medium sodium levels (Dmitrieva et al., 2023).
The study shows that people whose fasting serum sodium exceeds 142 mmol/l have increased risk to be biologically older, develop chronic diseases, and die at a younger age. This threshold can be used in clinical practice to identify people at risk. Since decreased hydration is one of the main factors that elevates serum sodium, the results are consistent with the hypothesis that decreased hydration may accelerate aging.
The authors cautioned that the data are observational, precluding cause-and-effect conclusions.
The National Academies of Medicine advises that women consume 6-9 cups (1.5-2.2 liters) and men consume 8-12 cups (2-3 liters) daily. There are 8 ounces in a cup. Fluids can also come from fruits, juices, and vegetables. These ranges have to be adjusted for exercise, health conditions (e.g., heart failure), and temperature (Agostoni et al., 2010; Dmitrieva et al., 2022).
Key Takeaways: Nutrition, Hydration, and Exercise
Nutrition, hydration, and physical exercise are essential components of stress management. Stress can deplete B vitamins, calcium, and magnesium. Clients should minimize caffeine and alcohol while emphasizing fiber-rich foods, healthy fats, and regular fish consumption. Physical activity confers a 35% reduction in cardiovascular mortality risk, with benefits beginning at just 7,000 steps per day. Exercise releases exerkines that improve metabolism, cardiovascular health, and cognitive function. Well-hydrated adults are more likely to experience healthy aging, with serum sodium levels above 142 mmol/l associated with increased biological aging risk.
Comprehension Questions: Lifestyle Factors
- What nutrients may become depleted during chronic stress, and why?
- According to research, what step count marks a significant reduction in mortality risk?
- What are exerkines, and how do they mediate the health benefits of exercise?
- How might physical exercise protect the aging brain, according to BDNF research?
Cutting Edge Topics in Relaxation
Ultra-Processed Foods: A Rising Health Threat
Ultra-processed foods represent a rising health threat. They constitute about 60 percent of calories consumed by Americans. In a paradigm shift, researchers increasingly focus on how producers process food in addition to calories, food pyramid position, and nutrients (O'Connor, 2022).
At their core, they are industrial concoctions containing a multitude of additives: salt, sugar and oils combined with artificial flavors, colors, sweeteners, stabilizers and preservatives. Typically they're subjected to multiple processing methods that transform their taste, texture and appearance into something not found in nature. Think Frosted Flakes, Hot Pockets, doughnuts, hot dogs, cheese crackers and boxed macaroni & cheese.
These hyper-palatable products combine artificial flavors, fat, sodium, and sugar to hijack the mesolimbic reward system, increase craving, and trigger overeating. The National Institutes of Health compared the effects of 2 weeks of ultra-processed meals with homemade meals. The meals contained identical fat, fiber, sodium, and sugar. When participants received ultra-processed meals, they ate 500 more calories per day and rapidly increased body fat and weight. The same individuals lost weight and reduced cholesterol when eating meals made from scratch. Appetite-suppressing PYY hormone levels rose and hunger-producing ghrelin levels fell (Hall et al., 2019; O'Connor, 2022).
Yet in dozens of large studies, scientists have found that ultra-processed foods are linked to higher rates of obesity, heart disease, hypertension, type 2 diabetes, and colon cancer. A recent study of more than 22,000 people found that people who ate a lot of ultra-processed foods had a 19 percent higher likelihood of early death and a 32 percent higher risk of dying from heart disease compared with people who ate few ultra-processed foods.

Chrono-Nutrition: When You Eat Matters
Research on the timing of meals suggests that we should consume the majority of our calories earlier, frontloading with a large breakfast and middle-sized lunch. Dinner should be the smallest meal, ideally at 4 pm. Benefits include weight loss, and improved blood sugar, cholesterol, and insulin sensitivity (Vujovic et al., 2022; Young et al., 2022).
O'Connor (2023) explained the scientific basis of chrono-nutrition. Scientists have uncovered several mechanisms that explain why an early-eating schedule is better for your health. Our bodies are better able to secrete insulin, a hormone that controls blood sugar levels, in the morning. We also tend to be more insulin-sensitive early in the day, meaning our muscles are better able to absorb and utilize glucose from our bloodstreams. But as the day progresses, we become less and less insulin-sensitive. By nighttime, the beta cells in the pancreas that produce insulin become sluggish and less responsive to blood sugar.
Exercise Effects on the Brain
Animal research has revealed that exercise triggers a cascade of neuroprotective changes. Physical activity increases expression of brain-derived neurotrophic factor (BDNF), which promotes neurogenesis and enhances learning (Gomez-Pinilla et al., 2001; Van Praag et al., 1999). Exercise also activates the gene coding for irisin, a hormone that may mediate cognitive benefits—mice lacking irisin showed impaired spatial learning compared to exercising wild-type mice (Islam et al., 2021). In Alzheimer's-prone mice, runners accumulated half the beta-amyloid plaques of sedentary controls (Adlard et al., 2005; Berchtold et al., 2005). Exercise may also boost glial cell-derived neurotrophic factor, protecting dopaminergic neurons from Parkinson's-like damage (Zigmond & Cotman, 2005), and reprogram microglia to resist neuroinflammation that compromises memory (Mee-Inta et al., 2019).
Human studies support these findings. In a two-year trial, 40% of paralyzed clients who exercised with electrode-equipped bikes regained motor function, compared to just 4% who only stretched (McDonald et al., 2002). A six-year study of 1,740 adults over 65 linked moderate exercise to reduced dementia incidence (Brownlee, 2006).
The Calming Signals of Beige Fat
While fat is often viewed through a negative lens, recent research suggests that not all adipose tissue is "nasty". Beyond the energy-storing white fat and heat-generating brown fat, scientists have identified beige fat, or inducible brown fat, which can perform both roles. A groundbreaking study published in Science reveals that these beige cells, clustered around major arteries, act as an endocrine organ by sending chemical signals that help blood vessels relax. In mouse models, the absence of this specialized tissue led to hypersensitivity to hormones that constrict vessels, resulting in significantly higher blood pressure. This discovery highlights a vital, "soothing" communication line between our fat and our vasculature (Brookshire, 2026).
These findings have profound implications for human health, as genetic variations in beige fat expression are linked to hypertension in people. By analyzing data from over 200,000 individuals, researchers found that those with specific protein variants controlling beige fat were more likely to suffer from high blood pressure and enlarged heart ventricles. Interestingly, the protective effects of this tissue appear to vary by sex, with male mice showing a more substantial impact than females. As scientists further investigate enzymes like QSOX1 regulated by these cells, they hope to unlock new therapeutic targets to manage cardiovascular disease. Ultimately, this research shifts the narrative from simply having fat to ensuring that the fat we have is functioning effectively.
The Science of Flexibility: Rethinking the Stretch
Modern fitness research is dismantling long-held gym myths, revealing that many common stretching practices are actually counterproductive. An international consensus of experts now clarifies that stretching does not reduce overall injury risk, and performing static stretching on "cold" muscles can actually lead to harm. Instead, athletes should prioritize a warm-up of light aerobic activity followed by dynamic stretching that simulates their specific workout. Interestingly, the "tightness" felt after skipping a session isn't the muscle physically shortening, but rather the nervous system entering a protective neurological state. By understanding that stretching primarily trains the brain to tolerate a greater range of motion, individuals can approach flexibility with more biological accuracy (Colino, 2026).
Effective stretching requires a personalized approach rather than a one-size-fits-all routine. While holding a static stretch for 10 to 30 seconds is standard for most, adults over 65 often require longer durations to see benefits due to slower-responding connective tissue. Furthermore, dynamic stretching has proven more effective than static holds for improving balance because it enhances neuromuscular coordination and sensory reaction to movement. It is also crucial to avoid "bouncing" or ballistic stretching, which can cause muscles to contract and strain rather than relax. Ultimately, the goal is to reach a point of mild discomfort without crossing into significant pain, ensuring the tissue remains stable and functional.
Comprehension Questions: Cutting Edge Topics
- How do ultra-processed foods affect appetite-regulating hormones, and what are the implications for weight management?
- According to chrono-nutrition research, why is eating earlier in the day potentially better for metabolic health?
- What serum sodium threshold did researchers identify as a marker for increased biological aging risk?
- How might a biofeedback practitioner incorporate nutrition and hydration counseling into a stress management program?
Glossary
abbreviated relaxation exercises: procedures like Stroebel's Quieting Response (QR) that produce low-to-moderate subjective and physiological change involve minimal sensory restriction, and are practiced for very brief periods. They are designed to replace symptoms like anxiety with more adaptive behaviors like cultivated low arousal or mindfulness.active volition: a process where you direct yourself to act like clenching a fist triggered by words like make or try.
add-on intervention: a therapeutic technique used in combination with standard care or another primary treatment rather than as a standalone intervention.
adipocytes: specialized cells that compose adipose tissue and are primarily responsible for storing or burning fat.
analgesia: insensitivity to pain.
angiotensinogen: a precursor to a hormone that causes blood vessels to constrict, thereby raising blood pressure.
autogenic discharges: Luthe identified 53 categories of side effects like tingling and muscle twitches in 100 novice clients.
autogenic meditation exercises: in autogenic training, these techniques teach visual imagery skills after mastering the six standard exercises.
autogenic modification procedures: in autogenic training, organ-specific formulae and intentional formulae are used when a client does not respond to the six standard exercises.
autogenic shift: in autogenic training, the transition to a passive, pre-sleep, hypnagogic autogenic state.
autogenic training: a deep relaxation procedure developed by Schultz and Luthe that involves six standard exercises, autogenic modification, and autogenic meditation.
ballistic stretching: a technique involving bouncing movements while stretching, which can be counterproductive or cause injury.
beige fat: also known as inducible brown fat, these cells are interspersed within white fat and can either store or burn energy depending on conditions.
brain-derived neurotrophic factor (BDNF): a member of the neurotrophin family that increases the number of new neurons and neural connectivity, whose expression is increased by exercise.
chrono-nutrition: the scientific study of the relationship between the timing of eating, circadian rhythms, and health.
clinically standardized meditation (CSM): a systematic secular meditative procedure that incorporates components from meditative techniques like TM.
deep relaxation procedures: procedures like Autogenic Training, meditation, and Progressive Relaxation that may require 15 minutes to several hours, involve a break from routine activity, and profoundly reduce physiological arousal and reset physiological activity to healthier values.
delayed onset muscle soreness (DOMS): the natural response of sore muscle fibers following a difficult workout.
differential relaxation: in progressive relaxation, the inhibition of unneeded muscle groups during routine activities.
dynamic stretching: movement-based stretching that takes joints and muscles through a full range of motion at a controlled pace.
empirical approach: data-guided strategy in which a therapist presents several procedures to a client, determines which procedure they prefer, and monitors subjective cognitive and physiological changes.
endocrine organ: a collection of tissues or cells that produce and release hormonal signals to regulate various bodily functions.
exerkines: a group of signaling molecules released during exercise that plays a crucial role in mediating its systemic benefits, including improved metabolism, cardiovascular health, and cognition.
foam roller: a dense cylindrical tool used after workouts to move fluid and inflammation away from sore areas.
glial cell-derived neurotrophic factor: a small protein synthesized in response to exercise, that promotes dopaminergic and motoneuron survival.
guided imagery: a structured form of visualization in which a practitioner or recording directs the client through a specific imagined scenario to promote relaxation, reduce anxiety, or manage pain.
habit: a behavior pattern often acquired through frequent repetition.
heaviness and warmth standard exercises: in autogenic training, exercises that teach clients the first two relaxation themes, heaviness and warmth, are divided into seven parts.
heritability index: the percentage of variation due to genetic influences.
high-density lipoproteins (HDL): a protective lipoprotein increased by exercise and moderate alcohol consumption.
hypnosis: a procedure that can aid therapy, for example, hypnotically-assisted psychotherapy.
hypnotherapy: a controversial term that implies that hypnosis is a therapy like cognitive behavior therapy.
hypnotic induction: from Hilgard's perspective, the promotion of an altered state of consciousness termed a hypnotic state.
hypnotic suggestibility: responsiveness to suggestion, measured by instruments like the Stanford Hypnotic Susceptibility Scale, appears to be distributed along a bell-shaped curve.
immersive virtual reality (IVR): a technology that uses headsets displaying 360-degree environments to create a sense of presence in a virtual world, increasingly used to enhance guided imagery and relaxation interventions.
intentional formulae: in autogenic training, autogenic modification procedures, which may be reinforcing or neutralizing, are used to increase or decrease behaviors.
irisin: a hormone expressed during exercise linked to learning and spatial memory in mice.
low-density lipoproteins (LDL): a potentially harmful form of lipoprotein, especially when the particles are small, is decreased by exercise and moderate alcohol consumption.
microglia: primary central nervous system immune cells that modulate neuroinflammation.
negative hallucination: a hypnotic phenomenon where normal perception is suppressed, for example, perceiving an audience as naked following a hypnotic suggestion.
organ-specific formulae: in autogenic training, autogenic modification procedures that modify standard exercise themes. For example, "My back is warm" instead of "My right arm is warm.""
osteoporosis: decreased bone density, is reduced by weight-bearing exercise that remodels the skeleton's bones.
passive attitude: in autogenic training, allowing is the most crucial element of the six standard exercises.
passive concentration: in autogenic training, the absence of effort and goal direction.
passive volition: in autogenic training, visualizing the desired change and then allowing the body to make the change at its own pace.
passive stretching: a method where a trained professional or outside force physically guides an individual into deeper stretches.
PRDM16: a specific protein that controls the identity and development of beige fat cells.
Quieting Response (QR): Stroebel's (1982) 6-second exercise instructs a client to focus on a stress cue, smile inwardly, take an easy deep breath, and let the jaw, tongue, and shoulders go limp as they exhale.
random-dot stereograms: hidden three-dimensional images created by repeating patterns within one image that can be perceived by allowing your eyes to defocus until you see double.
Relaxation state (R-state): a positive psychological state experienced during relaxation.
Relaxation-induced negative reactions (RINRs): anxiety experienced during relaxation training.
response stereotypy: a person's unique response pattern to stressors of identical intensity.
self-efficacy: an individual's expectancy that she can influence her outcomes. This concept overlaps with locus of control, mastery, and perceived control.
self-hypnosis: self-suggestion.
six relaxation themes: in autogenic training, the themes include heaviness, warmth, cardiac regulation, respiration, abdominal warmth, and forehead cooling.
six standard exercises: in autogenic training, exercises that focus on the physiological changes of the six relaxation themes. While the heaviness and warmth exercises are divided into seven parts, the remaining four exercises focus on only one body region (heart, lungs, abdomen, and forehead).
Stanford Hypnotic Susceptibility Scales: instruments that measure hypnotizability.
static stretching: the act of holding a specific position to the point of mild discomfort for a set period.
systematic desensitization: Wolpe's behavior therapy technique incorporates an abbreviated version of progressive relaxation.
taking back procedures: in autogenic training, standard exercises end with vigorous flexing of the arms, deep breathing, and opening the eyes, and the suggestion, "Arms firm, breathe deeply, open eyes."
Transcendental meditation (TM): mantric meditation developed by Maharishi Mahesh Yogi, in which an individual repeats Sanskrit syllables that have been assigned by an instructor based on age or personality.
transfer of training: generalization from clinic to a client's environment.
triglycerides: a potentially harmful form of lipoprotein that is decreased by exercise and increased by alcohol consumption.
ultra-processed foods: industrial foods containing artificial flavors, colors, oils, preservatives, salt, stabilizers, sweeteners, and sugar.
visualization: the generation of mental imagery, which can be somatosensory and visual, is a common element in interventions ranging from autogenic training to behavior therapy.
Test Yourself
Click on the ClassMarker logo to take 10-question tests over this unit without an exam password.
REVIEW FLASHCARDS ON QUIZLET
Click on the Quizlet logo to review our chapter flashcards.
Visit the BioSource Software Website
BioSource Software offers Human Physiology, which satisfies BCIA's Human Anatomy and Physiology requirement, and Biofeedback100, which provides extensive multiple-choice testing over BCIA's Biofeedback Blueprint.
Assignment
Now that you have completed this unit, think about the reason you incorporate specific relaxation exercises in your practice. What do you expect each to accomplish? Do they reliably achieve these goals? How do you encourage client practice?References
Achterberg, J. (1994). Rituals of healing: Using imagery for health and wellness. Bantam.
Adlard, P. A., Perreau, V. M., Pop, V., & Cotman, C. W. (2005). Voluntary exercise decreases amyloid load in a transgenic model of Alzheimer's Disease. The Journal of Neuroscience, 25(17), 4217-4221. https://doi.org/10.1523/JNEUROSCI.0496-05.2005
Agostoni, C. V., Bresson, J. L., Fairweather Tait, S., Flynn, A., Golly, I., Korhonen, H., Lagiou, P., Livik, M., Marchelli, R., Martin, A., & Moseley, B. (2010). Scientific opinion on dietary reference values for water.
Barber, J. (1996). A brief introduction to hypnotic analgesia. In J. Barber (Ed.), Hypnosis and suggestion in the treatment of pain: A clinical guide. Norton.
Barber, T. X. (1982). Hypnosuggestive procedures in the treatment of clinical pain: Implications for theories of hypnosis and suggestive therapy. In T. Millon, C. J. Green, & R. B. Meagher (Eds.), Handbook of clinical health psychology. Plenum.
Benson, H. (1975). The relaxation response. Morrow.
Berchtold, N. C., Chinn, G., Chou, M., Kesslak, J. P., & Cotman, C. W. (2005). Exercise primes a molecular memory for brain-derived neurotrophic factor protein induction in the rat hippocampus. Neuroscience, 133, 853-861. https://doi.org/10.1016/j.neuroscience.2005.03.026.
Brannon, L., Feist, J., & Updegraff, J. A. (2022). Health psychology (10th ed.). Cengage Learning.
Breznoscakova, D., Kovanicova, M., Sedlakova, E., & Pallayova, M. (2023). Autogenic training in mental disorders: What can we expect? International Journal of Environmental Research and Public Health, 20(5), 4344. https://doi.org/10.3390/ijerph20054344
Brookshire, B. (2026, January 15). This little-known type of fat may actually protect your heart. National Geographic.
Budzynski, T. (1994). The new frontier. Megabrain Report, 3, 58-65.
Carrington, P. (1999). Clinically standardized meditation (CSM) instructor's kit. Pace Educational Systems.
Carrington, P., & Lehrer, P. M. (2021). Modern forms of mantra meditation for stress management. In P. M. Lehrer & R. L. Woolfolk (Eds.), Principles and practice of stress management (4th ed.). The Guilford Press.
Colino, S. (2026, January 23). You might be stretching the wrong way, scientists say. National Geographic.
Dmitrieva, N. I., Gagarin, A., Liu, D., Wu, C. O., & Boehm, M. (2023). Middle-age high normal serum sodium as a risk factor for accelerated biological aging, chronic diseases, and premature mortality. eBioMedicine, 104404.
Dmitrieva, N. I., Rosing, D. R., & Boehm, M. (2022). Making decision about fluid intake: increase or not increase. European Heart Journal, 43(41), 4438-4439. https://doi.org/10.1093/eurheartj/ehac368
Freedman, R. R., Ianni, P., & Wenig, P. (1983). Behavioral treatment of Raynaud's disease. Journal of Consulting and Clinical Psychology, 51(4), 539-549. https://doi.org/10.1037//0022-006x.51.4.539
Fung, T. T., Willett, W. C., Stampfer, M. J., Manson, J. E., & Hu, F. B. (2001). Dietary patterns and the risk of coronary heart disease in women. Archives of Internal Medicine, 161(15), 1857-1862. https://doi.org/10.1001/archinte.161.15.1857
Gard, T., Hölzel, B. K., & Lazarm S. W. (2014). The potential effects of meditation on age-related cognitive decline: A systematic review. Annals of the New York Academy of Sciences, 1307(1), 89-103. https://doi.org/10.1111/nyas.12348
Gomez-Pinilla, F., Ying, Z., Opazo, P., Roy, R. R., & Edgerton, V. R. (2001). Differential regulation by exercise of BDNF and NT-3 in rat spinal cord and skeletal muscle. Eur J Neurosci, 13, 1078-84. https://doi.org/10.1046/j.0953-816x.2001.01484.x
Gurung, R. A. R. (2018). Health psychology: Well-being in a diverse world (4th ed.). Thompson Wadsworth.
Hall, K. D., Ayuketah, A., Brychta, R., Cai, H., Cassimatis, T., Chen, K. Y., Chung, S. T., Costa, E., Courville, A., Darcey, V., Fletcher, L. A., Forde, C. G., Gharib, A. M., Guo, J., Howard, R., Joseph, P. V., McGehee, S., Ouwerkerk, R., Raisinger, K., Rozga, I., … Zhou, M. (2019). Ultra-processed diets cause excess calorie intake and weight gain: An inpatient randomized controlled trial of ad libitum food intake. Cell metabolism, 30(1), 67, 77.e3. https://doi.org/10.1016/j.cmet.2019.05.008
Hilgard, E. R. (1978). Hypnosis and pain. In R. A. Sternbach (Ed.). The psychology of pain. Raven Press.
Hölzel, B. K., Carmody, J., Evans, K. C., Hoge, E. A., Dusek, J. A., Morgan, L., Pitman, R. K., & Lazar, S. W. (2009). Stress reduction correlates with structural changes in the amygdala. Social Cognitive and Affective Neuroscience, 5(1), 11-17. https://doi.org/10.1093/scan/nsp034
Institute of Medicine of the National Academies (2005). Water. Dietary reference intakes for water, potassium, chloride, and sulfate. The National Academies Press.
Islam, M. R., Valaris, S., Young, M. F., Haley, E. B., Luo, R., Bond, S. F., Mazuera, S., Kitchen, R. R., Caldarone, B. J., Bettio, L. E. B., Christie, B. R., Schmider, A. B., Soberman, R. J., Besnard, A., Jedrychowski, M. P., Kim, H., Tu, H., Kim, E., Choi, S. H., Tanzi, R. E., Spiegelman, B. M., & Wrann, C. D. (2021). Exercise hormone irisin is a critical regulator of cognitive function. Nature Metabolism, 3, 1058-1070. https://doi.org/10.1038/s42255-021-00438-z
Jacobs, A. L., Kurtz, R. M., & Strube, M. J. (1995). Hypnotic analgesia, expectancy effects, and choice of a design: A reexamination. International Journal of Clinical and Experimental Hypnosis, 43, 45-68. https://doi.org/10.1080/00207149508409375
Jacobson, E. (1929). Progressive relaxation: A physiological and clinical investigation of muscular states and their significance in psychology and medical practice. University of Chicago Press.
Jacobson, E. (1934). You must relax: A practical method of reducing the strains of modern living. Mc-Graw-Hill.
Jones, H. G., Rizzo, R. R. N., Pulling, B. W., Braithwaite, F. A., Grant, A. R., McAuley, J. H., Jensen, M. P., Moseley, G. L., Rees, A., & Stanton, T. R. (2024). Adjunctive use of hypnosis for clinical pain: A systematic review and meta-analysis. Pain Reports, 9(5), e1185. https://doi.org/10.1097/PR9.0000000000001185
Karlin, R. A. (2021). The treatment of pain and stress with hypnosis: A series of emerging literatures. In P. M. Lehrer & R. L. Woolfolk (Eds.), Principles and practice of stress management (4th ed.). The Guilford Press.
Kekecs, Z., Bowers, J., Johnson, A., Kendrick, C., & Elkins, G. (2016). The Elkins Hypnotizability Scale: Assessment of reliability and validity. Int J Clin Exp Hypn, 64, 285-304. https://doi.org/10.1080/00207144.2016.1171089
Khazan, I. (2019). Biofeedback and mindfulness in everyday life. W. W. Norton & Company.
Khedkar, S. (2025). Exerkines: Molecular messengers that mediate exercise effects. The Scientist. https://doi.org/10.1038/s41574-022-00641-2
Kirsch, I., & Lynn, S. (1995). The altered state of hypnosis: Changes in the theoretical landscape. American Psychologist, 50, 846-858. https://doi.org/10.1037/0003-066X.50.10.846
Kohlert, A., Wick, K., & Rosendahl, J. (2022). Autogenic training for reducing chronic pain: A systematic review and meta-analysis of randomized controlled trials. International Journal of Behavioral Medicine, 29(5), 531-542. https://doi.org/10.1007/s12529-021-10038-6
Kouhpayeh, M. S., Khezri, S., Goli, R., Faraji, N., Choobi Anzali, B., Maroofi, H., Hassanpour, A., & Nourazar, M. A. (2024). The effect of guided imagery on perioperative anxiety in hospitalized adult patients: A systematic review of randomized controlled trials. Surgery in Practice and Science, 18, 100255. https://doi.org/10.1016/j.sipas.2024.100255
Kral, T., Davis, K., Korponay, C., Hirshberg, M. J., Hoel, R., Tello, L. Y., Goldman, R. I., Rosenkranz, M. A., Lutz, A., & Davidson, R. J. (2022). Absence of structural brain changes from mindfulness-based stress reduction: Two combined randomized controlled trials. Science advances, 8(20), eabk3316. https://doi.org/10.1126/sciadv.abk3316
Kristeller, J. L. (2021). Mindfulness meditation for stress management. In P. M. Lehrer & R. L. Woolfolk (Eds.), Principles and practice of stress management (4th ed.). The Guilford Press.
Lazar, S. W., Kerr, C. E., Wasserman, R. H., Gray, J. R., Greve, D. N., Treadway, M. T., McGarvey, M., Quinn, B. T., Dusek, J. A., Benson, H., Rauch, S. L., Moore, C. I., & Fischl, B. (2005). Meditation experience is associated with increased cortical thickness. Neuroreport, 16(17), 1893. PMID: 16272874
Lehrer, P., & Carrington, P. (2003). Progressive relaxation, autogenic training, and meditation. In D. Moss, A. McGrady, T. C. Davies, & I. Wickramasekera (Eds.), Handbook of mind-body medicine for primary care. Sage Publications.
Lichstein, K. L. (1988). Clinical relaxation strategies. John Wiley & Sons.
Linden, W. (1990). Autogenic training: A clinical guide. The Guilford Press.
Linden, W. (1994). Autogenic training: A narrative and a meta-analytic review of outcome. Biofeedback and Self-Regulation, 19, 227-264. https://doi.org/10.1007/BF01721069
Linden, W. (2021). The autogenic training method of J. H. Schultz. In P. M. Lehrer & R. L. Woolfolk (Eds.), Principles and practice of stress management (4th ed.). The Guilford Press.
Li, W. W., Nannestad, J., Leow, T., & Heward, C. (2024). The effectiveness of mindfulness-based stress reduction (MBSR) on depression, PTSD, and mindfulness among military veterans: A systematic review and meta-analysis. Health Psychology Open, 11(2). https://doi.org/10.1177/20551029241302029
Ludwig, D. S., Pereira, M. A., Kroenke, C. H., Hilner, J. E., Van Horn, L., Slattery, M., & Jacobs, D. R. Jr. (1999). Dietary fiber, weight gain, and cardiovascular risk factors in young adults. Journal of the American Medical Association, 282(16), 1539-1546. https://doi.org/10.1001/jama.282.16.1539
Lutz, A., Jha, A. P., Dunne, J. D., & Saron, C. D. (2015). Investigating the phenomenological matrix of mindfulness-related practices from a neurocognitive perspective. American Psychologist, 70(7), 632-658. https://doi.org/10.1037/a0039585
Lynn, S. J,, Laurence, J.-R., & Kirsch, I. (2015). Hypnosis, suggestion, and suggestibility: An integrative model. Am J Clin Hypn, 57, 314-29. https://doi.org/10.1080/00029157.2014.976783
McDonald, J. W. (2004). Repairing the damaged spinal cord: From stem cells to activity-based restoration therapies. Clinical Neurosurgery, 51, 207-227. PMID: 15571147
McDonald, J. W., Becker, D., Sadowsky, C. L., Jane, J. A., Conturo, T. E., & Schultz, L. M. (2002). Late recovery following spinal cord injury. Journal of Neurosurgery, 97, 252-265.https://doi.org/10.3171/spi.2002.97.2.0252
McGuigan, F. M., & Lehrer, P. M. (2021). Progressive relaxation: Origins, principles, and clinical applications. In P. M. Lehrer & R. L. Woolfolk (Eds.), Principles and practice of stress management (4th ed.). The Guilford Press.
Mee-Inta, O., Zhao, Z.-W., & Kuo, Y.-M. (2019). Physical exercise inhibits inflammation and microglial activation. Cells, 8(7), 691. https://doi.org/10.3390/cells8070691
Miller, M. F., Barabasz, A. F., & Barabasz, M. (1991). Effects of active alert and relaxation hypnotic inductions on cold pressor pain. Journal of Abnormal Psychology, 100, 223-226. https://doi.org/10.1037//0021-843x.100.2.223
Montgomery, G. H., Bovbjerg, D. H., Schnur, J. B., David, D., Goldfarb, A., Weltz, C. R., Schechter, C., Graff-Zivin, J., Tatrow, K., Price, D. D., & Silverstein, J. H. (2007). A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery patients. J Natl Cancer Inst, 99(17), 1304-1312. https://doi.org/10.1093/jnci/djm106
Montgomery, G. H,, David, D., Winkel. G., Silverstein, J. H., & Bovbjerg, D. H. (2002). The effectiveness of adjunctive hypnosis with surgical patients: A meta-analysis. Anesth Analg, 94(6), 1639-1645, table of contents. https://doi.org/10.1097/00000539-200206000-00052
Montgomery, G. H., DuHamel, K. N., & Redd, W. H. (2000). A meta-analysis of hypnotically induced analgesia: How effective is hypnosis? International Journal of Clinical and Experimental Hypnosis, 48, 138-153. https://doi.org/10.1080/00207140008410045
Morgan, A. H. (1973). The heritability of hypnotic susceptibility in twins. J Abnorm Psychol, 82, 55-61. https://doi.org/10.1037/h0034854
Moss, D. (2004). Adjunctive interventions and assessment. In A. Crider & D. D. Montgomery (Eds.), Introduction to biofeedback. Association for Applied Psychophysiology and Biofeedback.
Moss, D. (2020). Biofeedback-assisted relaxation training: A clinically effective treatment protocol. Biofeedback, 48(2), 32-40. https://doi.org/10.5298/1081-5937-48.02.02
Moss, D., & Willmarth, E. (2019). Hypnosis, anesthesia, pain management, and preparation for medical procedures. Ann Palliat Med, 8(4), 498-503. https://doi.org/10.21037/apm.2019.07.01
Muhammad Khir, S., Wan Mohd Yunus, W. M. A., Mahmud, N., Wang, R., Panatik, S. A., Sukor, M. S. M., & Nordin, N. A. (2024). Efficacy of progressive muscle relaxation in adults for stress, anxiety, and depression: A systematic review. Psychology Research and Behavior Management, 17, 345-365. https://doi.org/10.2147/PRBM.S437277
Nash, J., Stockdale, S., & Hoffman, D. A. (2001). Question: Have you seen any negative effects associated with EEG neurofeedback? Journal of Neurofeedback, 4, 65-69.
Nash, M. R. (2001, July). The truth and the hype of hypnosis. Scientific American, 285, 47-55. PMID: 11432194
Noetel, M., Sanders, T., Gallardo-Gómez, D., Taylor, P., Del Pozo Cruz, B., van den Hoek, D., Smith, J. J., Mahoney, J., Spathis, J., Moresi, M., Pagano, R., Pagano, L., Vasconcellos, R., Arnott, H., Varley, B., Parker, P., Biddle, S., & Lonsdale, C. (2024). Effect of exercise for depression: Systematic review and network meta-analysis of randomised controlled trials. BMJ, 384, e075847. https://doi.org/10.1136/bmj-2023-075847
O'Connor, A. (2022). What are ultra-processed foods? What should I eat instead? The Washington Post.
O'Connor, A. (2023). It's not just what you eat, but the time of day you eat it. The Washington Post.
Paluch, A. E., Gabriel, K. P., Fulton, J. E., Lewis, C. E., Schreiner, P. J., Sternfeld, B., Sidney, S., Siddique, J., Whitaker, K. M., & Carnethon, M. R. (2021). Steps per day and all-cause-mortality in middle-aged adults in the Coronary Artery Risk Development in Young Adults Study. JAMA Network Open, 4(9), e2124516. https://doi.org/10.1001/jamanetworkopen.2021.24516
Pan, Y., Li, F., Liang, H., Chen, L., Wang, J., Wei, W., Li, F., & Fu, D. (2024). Effectiveness of mindfulness-based stress reduction on mental health and psychological quality of life among university students: A GRADE-assessed systematic review. Evidence-Based Complementary and Alternative Medicine, 2024, 8872685. https://doi.org/10.1155/2024/8872685
Pardini, S., Gabrielli, S., Olivetto, S., Fusina, F., Dianti, M., Forti, S., & Lancini, S. (2024). Exploring virtual reality versus traditional guided imagery for reducing anxiety: A pilot randomized controlled trial. Cyberpsychology, Behavior, and Social Networking, 27(8), 596-605. https://doi.org/10.1089/cyber.2023.0594
Patterson, D. R. (2010). Clinical hypnosis for pain control. American Psychological Association.
Pelletier, K. R. (1977). Mind as healer, Mind as slayer. Dell Publishing Company, Incorporated.
Piccione, C., Hilgard, E. R., & Zimbardo, P. G. (1989). On the degree of stability of measured hypnotizability over a 25-year period. J Pers Soc Psychol, 56, 289-295. https://doi.org/10.1037//0022-3514.56.2.289
Rosendahl, J., Alldredge, C. T., & Haddenhorst, A. (2024). Meta-analytic evidence on the efficacy of hypnosis for mental and somatic health issues: A 20-year perspective. Frontiers in Psychology, 14, 1330238. https://doi.org/10.3389/fpsyg.2023.1330238
Schwartz, M. S. (2016). Intake decisions and preparation of patients for therapy. In M. S. Schwartz & F. Andrasik (Eds.). Biofeedback: A practitioner’s guide (4th ed.). The Guilford Press.
Schwartz, M. S., Schwartz, N. M., & Monastra, V. J. (2016). Problems associated with relaxation procedures and biofeedback, and guidelines for management. In M. S. Schwartz & F. Andrasik (Eds.). Biofeedback: A practitioner’s guide (4th ed.). The Guilford Press.
Seid, A. A., Mohammed, A. A., & Hasen, A. A. (2023). Progressive muscle relaxation exercises in patients with COVID-19: Systematic review and meta-analysis. Medicine, 102(14), e33464. https://doi.org/10.1097/MD.0000000000033464
Singh, B., Olds, T., Curtis, R., Dumuid, D., Virgara, R., Watson, A., Szeto, K., O'Connor, E., Ferguson, T., Eglitis, E., Miatke, A., Simpson, C. E., & Maher, C. (2023). Effectiveness of physical activity interventions for improving depression, anxiety and distress: An overview of systematic reviews. British Journal of Sports Medicine, 57(18), 1203-1209. https://doi.org/10.1136/bjsports-2022-106195
Smith, J. C. (1986). Meditation, biofeedback, and the relaxation controversy: A cognitive-behavioral perspective. American Psychologist, 41, 1007-1009.
Smith, J. C. (1990). Cognitive-behavioral relaxation training: A new system of strategies for treatment and assessment. Springer.
Smith, J. C. (1999). ABC relaxation theory. Springer.
Smith, J. C. (2001). Advances in ABC relaxation: Applications and inventories. Springer.
Smith, J. C. (2005). Relaxation, meditation, and mindfulness: A mental health professional's guide to new and traditional approaches. Springer.
Smith, J. C. (2007). The psychology of relaxation. In P. M. Lehrer, R. L. Woolfolk, & W. E. Sime (Eds.). Principles and practice of stress management (3rd ed.). The Guildford Press.
Smith, J. C. (2016). Relaxation today: Self-stressing and psychological relaxation theory. In M. S. Schwartz & F. Andrasik (Eds.). Biofeedback: A practitioner’s guide (4th ed.). The Guilford Press.
Smith, J. C. (2017). Stress and coping: The eye of mindfulness. Kendall Hunt
Smith, J. C. (2019). Third-generation mindfulness and the universe of relaxation. Kendall Hunt.
Smith, J. C. (2021). The psychology of relaxation. In P. M. Lehrer & R. L. Woolfolk (Eds.). Principles and practice of stress management (4th ed.). The Guildford Press.
Smith, J. C., Amutio, A., Anderson, J. P., & Aria, L. A. (1996). Relaxation: Mapping an uncharted world. Biofeedback and Self-Regulation, 21, 63-90. https://doi.org/10.1007/BF02214150
Smith, J. C., & Jackson, L. (2001). Breathing exercises and relaxation states. In J. C. Smith (Ed.), Advances in ABC relaxation: Applications and inventories (pp. 202-204). Springer.
Smith, J. C., & Joyce, C. A. (2004). Mozart vs. new age music: Relaxation states, stress, and ABC relaxation theory. Journal of Music Therapy, 41, 215-224. https://doi.org/10.1093/jmt/41.3.215
Smith, J. C., Wedell, A. B., Kolotylo, C. J., Lewis, J. E., Byers, K. Y., & Segin, C. M. (2000). ABC relaxation theory and the factor structure of relaxation states, recalled relaxation activities, dispositions, and motivations. Psychological Reports, 86, 1201-1208. https://doi.org/10.2466/pr0.2000.86.3c.1201
Stetter, F., & Kupper, S. (2002). Autogenic training: A meta-analysis of clinical outcome studies. Applied Psychophysiology and Biofeedback, 27, 45-98. https://doi.org/10.1023/a:1014576505223.
Striefel, S. (2004). Module 8: Professional conduct. In A. Crider and D. D. Montgomery (Eds.). Introduction to biofeedback: An AAPB independent study program. Association for Applied Psychophysiology and Biofeedback.
Taylor, S. (2021). Health psychology (10th ed.). McGraw Hill.
U.S. Department of Health and Human Services (USDHHS). (2018). Physical activity guidelines for Americans (2nd ed.), Washington, DC: Author.
Vaddadi, G. (2016). Cardiovascular risk factors: Role of lifestyle. In M. E. Alvarenga, & D. Byrne (Eds.). Handbook of psychocardiology. Springer Singapore.
Van Praag, H., Christie, B. R., Sejnowski, T. J., & Gage, F. H. (1999). Running enhances neurogenesis, learning, and long-term potentiation in mice. Proc Natl Acad Sci USA, 96, 13427, 13431. https://doi.org/10.1073/pnas.96.23.13427
Vujović, N., Piron, M. J., Qian, J., Chellappa, S. L., Nedeltcheva, A., Barr, D., Heng, S. W., Kerlin, K., Srivastav, S., Wang, W. & Scheer, F. A. (2022). Late isocaloric eating increases hunger, decreases energy expenditure, and modifies metabolic pathways in adults with overweight and obesity. Cell Metabolism, 34(10), 1486-1498.
Wickramasekera, I. (2003). The high risk model of threat perception and the Trojan Horse role induction: Somatization and psychophysiological disease. In D. Moss, A. McGrady, T. C. Davies, & I. Wickramasekera (Eds.), Handbook of mind-body medicine for primary care. Sage Publications.
Young, I. E., Poobalan, A., Steinbeck, K., O'Connor, H. T., & Parker, H. M. (2022). Distribution of energy intake across the day and weight loss: A systematic review and meta‐analysis. Obesity Review, e13537.
Zigmond, M. J., & Cotman, C. W. (2005). Exercise and central nervous system disease. Annual Meeting of the Society for Neuroscience.